Type B Adverse Drug Reaction: What You Need to Know About Unpredictable Medication Reactions
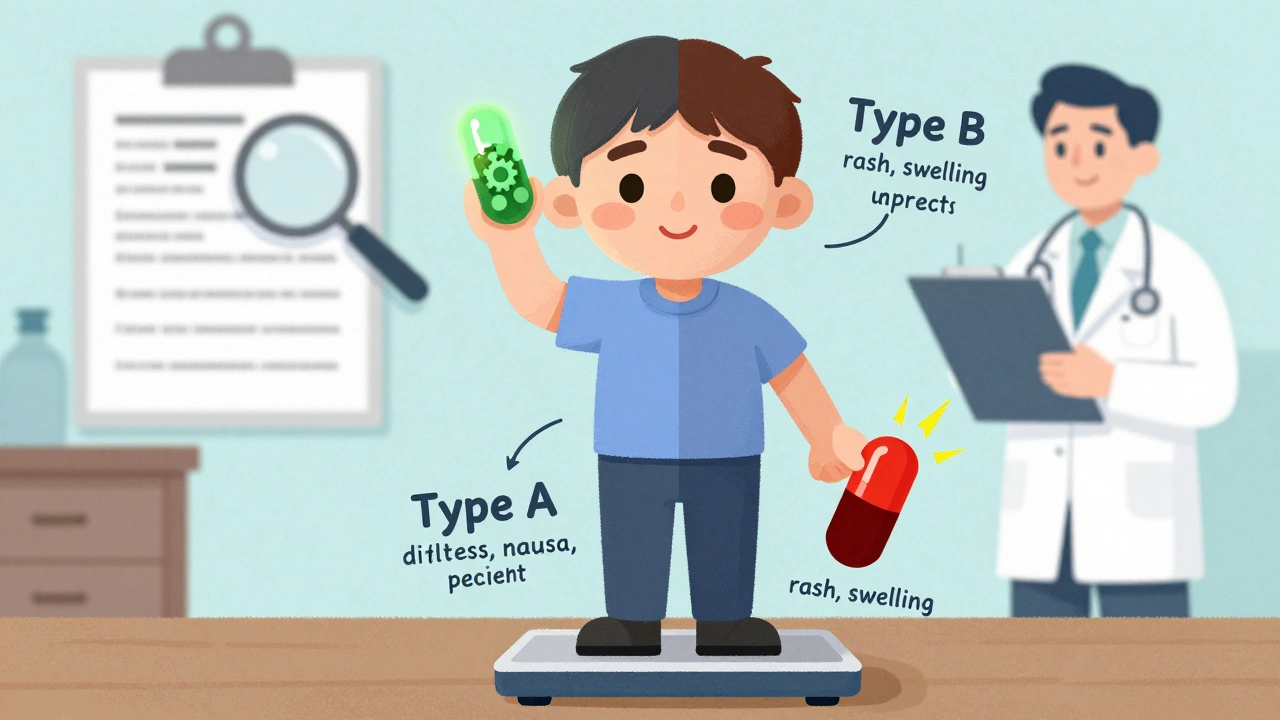
When a drug causes harm that no one saw coming—no matter the dose—that’s a Type B adverse drug reaction, an unpredictable, non-dose-dependent reaction to medication that isn’t an extension of the drug’s known pharmacological effects. Also known as idiosyncratic drug reactions, these events are rare, often serious, and can strike without warning—even in people who’ve taken the same drug safely for years. Unlike Type A reactions, which are predictable and linked to how the drug works in the body (like stomach upset from NSAIDs), Type B reactions are like a glitch in your immune system or metabolism. They’re not caused by too much of the drug. They’re caused by your body reacting to it in a way no one fully understands.
These reactions include drug hypersensitivity, a severe immune response triggered by certain medications, often involving rash, fever, or organ damage, and anaphylaxis, a life-threatening allergic reaction that can happen within minutes of taking a drug like penicillin or aspirin. They can also show up as liver failure from acetaminophen in people who don’t overdose, or severe skin reactions like Stevens-Johnson syndrome from sulfa drugs or anticonvulsants. These aren’t side effects you read about on a pill bottle. They’re surprises your body throws at you.
Some drugs are more likely to cause these reactions than others. Antibiotics like penicillin, anticonvulsants like carbamazepine, and allopurinol for gout top the list. Even common painkillers like ibuprofen can trigger them in people with asthma—something we see in posts about NSAID sensitivity and asthma. The risk isn’t always about how much you take. It’s about your genes, your immune history, and sometimes pure bad luck. That’s why these reactions are so hard to predict. No blood test can tell you ahead of time if you’re at risk.
What makes Type B reactions even trickier is that they often show up weeks after you start a new drug. You might think your rash or fever is from a cold, not your new blood pressure pill. That delay is why doctors miss them. But if you’ve had a strange reaction to one drug, you’re more likely to react to others—even if they’re in a different class. That’s why tracking every medication you take matters. It’s not just about what’s in your pill organizer. It’s about what your body remembers.
The posts below dig into real cases where drugs caused unexpected harm—and how patients and doctors figured it out. You’ll find stories about people reacting badly to antibiotics, antidepressants, and even common painkillers. We cover how to spot the warning signs, what to do if you think you’re having a reaction, and how to talk to your pharmacist about your personal risk. These aren’t theoretical warnings. They’re lessons from real people who lived through it.
- 14 Comments
Learn the key differences between Type A and Type B adverse drug reactions - why some side effects are common and predictable, while others are rare but dangerous. Understand how to recognize, prevent, and report them.
