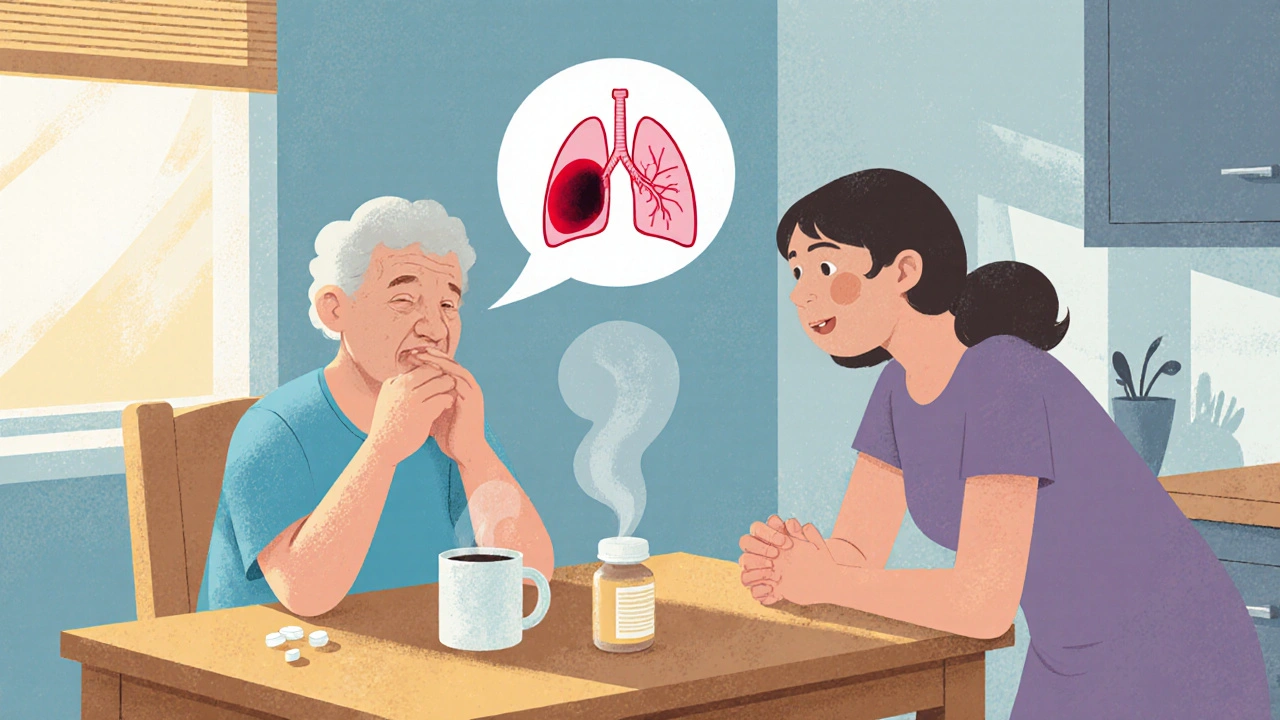
Pulmonary Embolism: What It Is and Why It Matters
When dealing with pulmonary embolism, a sudden blockage of a lung artery usually caused by a blood clot that traveled from elsewhere in the body. Also known as PE, it can quickly become life‑threatening if not recognized and treated. Deep vein thrombosis, the formation of clots in the deep veins of the legs or pelvis is the most common source of those clots, making the two conditions tightly linked. Understanding how anticoagulant therapy, medications that thin the blood to prevent further clotting works, and why CT pulmonary angiography, a specialized CT scan that visualizes the pulmonary arteries is the go‑to diagnostic test, gives you the tools to spot danger early.
How Pulmonary Embolism Connects to Other Health Issues
The first semantic connection is simple: pulmonary embolism encompasses the blockage of a lung artery, which often originates from a clot formed in deep veins. That means any factor that encourages clotting—like prolonged immobility, surgery, or certain genetic disorders—adds to the risk. Next, diagnosing the blockage requires imaging; the gold standard is CT pulmonary angiography, which captures real‑time images of the clot’s size and location. Finally, once a clot is confirmed, the treatment pathway pivots to anticoagulant therapy, which stops the clot from growing and prevents new clots from forming. These three entities—clot origin, imaging, and medication—form a logical chain that clinicians follow every day.
Risk factors are the next piece of the puzzle. Age over 60, obesity, smoking, and a history of cancer all raise the odds. Even everyday habits like long‑distance travel can trigger deep vein thrombosis, which may silently travel to the lungs. Knowing these triggers helps you gauge personal risk and take preventive steps, such as staying active, hydrating, or using compression stockings on long trips. The more you understand the risk landscape, the better you can work with your doctor to tailor a plan that lowers the chance of a PE.
Symptoms can be vague, which is why many people miss the warning signs. Sudden shortness of breath, sharp chest pain that worsens with breathing, rapid heartbeat, or a feeling of faintness are classic clues. Sometimes a cough produces blood‑streaked sputum. These signs overlap with other conditions, so a high index of suspicion is crucial. If you notice any of these symptoms after a risky event—like surgery or a marathon—seek medical help right away. Early detection via CT pulmonary angiography dramatically improves outcomes.
Once a diagnosis is made, anticoagulant therapy becomes the cornerstone of care. Traditional options include warfarin, which requires regular blood tests to keep the INR in range, and newer direct oral anticoagulants (DOACs) like apixaban or rivaroxaban, which need less monitoring. The choice depends on factors such as kidney function, drug interactions, and patient preference. For severe cases, clot‑busting drugs (thrombolytics) or surgical removal may be necessary, but these carry higher bleeding risks and are reserved for life‑threatening scenarios.
Long‑term follow‑up is another vital step. After the initial treatment phase, many patients continue on a lower‑dose anticoagulant for three to six months, sometimes longer if they have ongoing risk factors. Repeat imaging may be ordered to ensure the clot has resolved. Lifestyle adjustments—maintaining a healthy weight, exercising regularly, and quitting smoking—further reduce the chance of recurrence. Education about warning signs empowers patients to act quickly if symptoms return.
Behind the scenes, researchers are exploring innovative ways to prevent and treat pulmonary embolism. Newer biomarkers aim to detect clot formation earlier, while advanced imaging techniques promise clearer pictures with less radiation. At the same time, novel anticoagulants with fewer side effects are entering clinical trials. Staying informed about these developments can help you discuss cutting‑edge options with your healthcare provider.
All of these topics—risk factors, symptoms, imaging, medication, and future advances—interlock to give a full picture of pulmonary embolism. Below you’ll find a curated set of articles that dive deeper into each area, from how to recognize early warning signs to detailed comparisons of anticoagulant choices. Whether you’re a patient, a caregiver, or just curious about the condition, the collection offers practical insights you can use right now.
- 13 Comments
A clear, 2025‑updated guide for patients and families explaining pulmonary embolism symptoms, diagnosis, treatment options, home care, and prevention strategies.
