Anticoagulant Selection Guide
Understand Your Treatment Options
This tool helps you understand which anticoagulant medications might be appropriate based on your specific health factors. Always discuss treatment options with your healthcare provider.
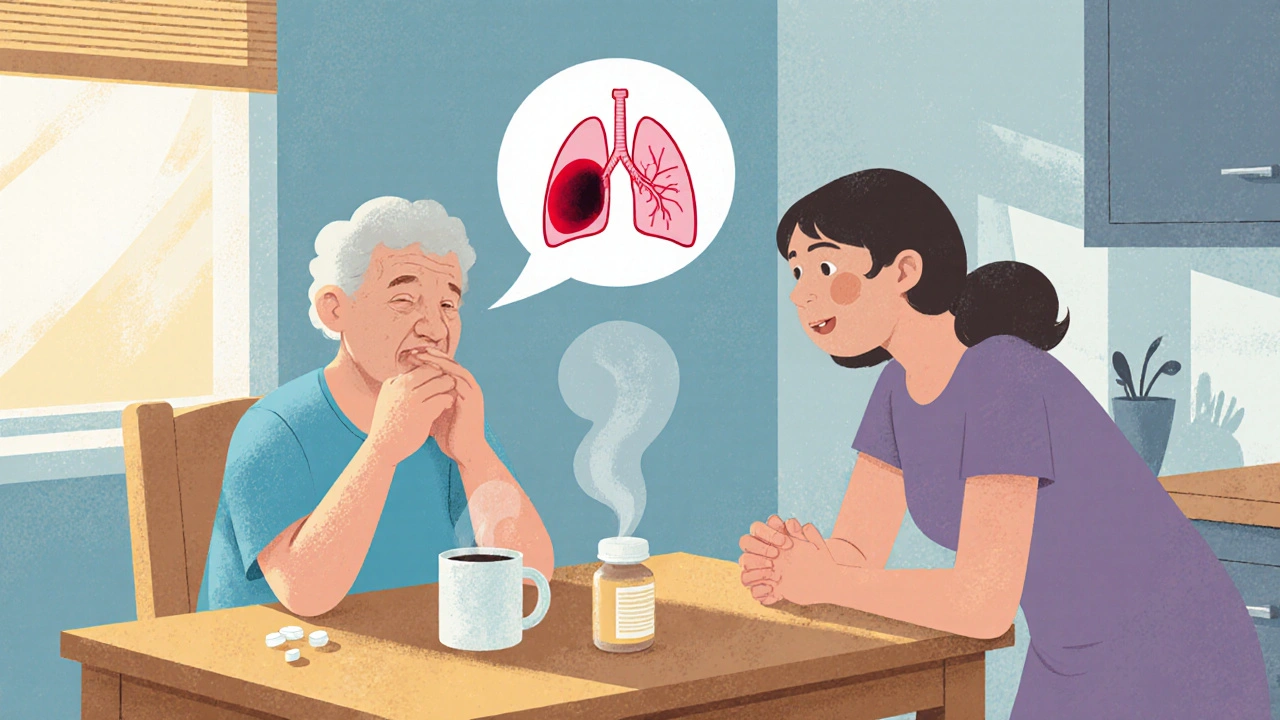
Medication Factors
When a Pulmonary Embolism is defined as a blockage in one of the lung arteries caused by a blood clot that has traveled from elsewhere in the body, it can feel like a medical nightmare for anyone involved. You might be sitting at the kitchen table with a loved one, trying to make sense of breathlessness, chest pain, or a sudden cough. This guide walks you through what actually happens, how doctors figure it out, and what steps you can take to treat and prevent it - all in plain language and up‑to‑date for 2025.
What Triggers a Blood Clot to Head to the Lungs?
Most Deep Vein Thrombosis (DVT) starts in the deep veins of the legs or pelvis. When a clot forms there, a piece can break off and travel through the venous system, the heart, and finally lodge in the pulmonary artery. This journey is why DVT and pulmonary embolism (PE) are often called venous thromboembolism (VTE) together.
Typical triggers include prolonged immobility (think long flights or bed rest after surgery), certain cancers, hormonal therapies, and inherited clotting disorders. Even something as simple as a recent knee replacement can boost the risk dramatically.
Spotting the Warning Signs
PE symptoms can vary wildly, but here are the most common clues you shouldn’t ignore:
- Sudden shortness of breath that gets worse with activity
- Sharp, stabbing chest pain that may worsen when you take a deep breath
- Rapid heartbeat (tachycardia)
- Light‑headedness or fainting
- Coughing up blood‑streaked sputum
If any of these appear out of the blue, especially after a recent surgery or a long journey, call emergency services right away. Early detection saves lives.
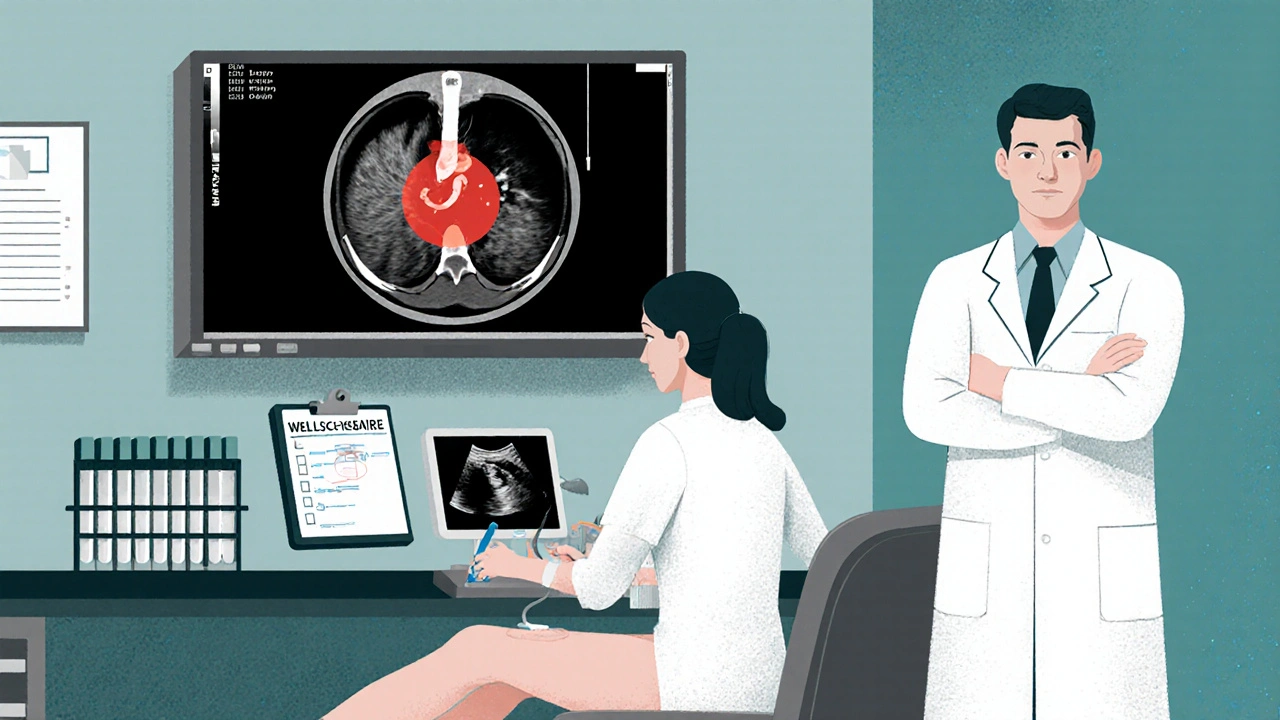
How Doctors Confirm the Diagnosis
The diagnostic pathway blends clinical judgment with imaging and lab tests. Here’s the typical flow:
- Clinical assessment: Doctors use the Wells score or the revised Geneva score to estimate the probability of PE based on symptoms and risk factors.
- D‑dimer test: A blood test that measures clot‑breakdown products. A low D‑dimer can rule out PE in low‑risk patients.
- Imaging:
- CT Pulmonary Angiography (CTPA) is the gold‑standard - it shows the clot directly.
- Ventilation‑Perfusion (V/Q) scan is used when radiation exposure is a concern.
- Compression ultrasound of the legs can detect DVT, supporting a PE diagnosis.
- Echocardiography: In severe cases, an echo can reveal right‑heart strain caused by the clot.
These tools together give a clear picture of where the clot sits and how big the threat is.
Treatment Options: From Hospital to Home
Once PE is confirmed, the goal is to stop the clot from growing, prevent new clots, and manage symptoms. Treatment usually falls into three categories:
- Anticoagulant therapy: Blood thinners that stop further clotting.
- Thrombolytic therapy: Clot‑busting drugs reserved for massive PE with heart strain.
- Mechanical interventions: Catheter‑directed clot removal or surgical embolectomy in rare, life‑threatening cases.
Most patients start on an injectable anticoagulant (like low‑molecular‑weight heparin) in the emergency department, then transition to an oral option for long‑term management.
Choosing the Right Anticoagulant - A Quick Comparison
| Medication | Mechanism | Typical Duration | Monitoring Needed | Key Considerations |
|---|---|---|---|---|
| Warfarin | Vitamin K antagonist | 3-12 months or indefinite | INR checks 2-3×/week initially | Dietary vitamin K interactions, many drug interactions |
| Apixaban | Direct Factor Xa inhibitor | 3-12 months or indefinite | No routine labs | Renal dosing needed, less bleed risk than warfarin |
| Rivaroxaban | Direct Factor Xa inhibitor | 3-12 months or indefinite | No routine labs | Once‑daily dosing, caution with hepatic impairment |
| Dabigatran | Direct thrombin inhibitor | 3-12 months or indefinite | No routine labs | Requires a 5‑day lead‑in with heparin, GI side‑effects |
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban have become first‑line for most PE patients because they avoid the frequent blood tests that warfarin demands. However, warfarin remains useful for people with severe kidney disease or those already on medications that interact with DOACs.
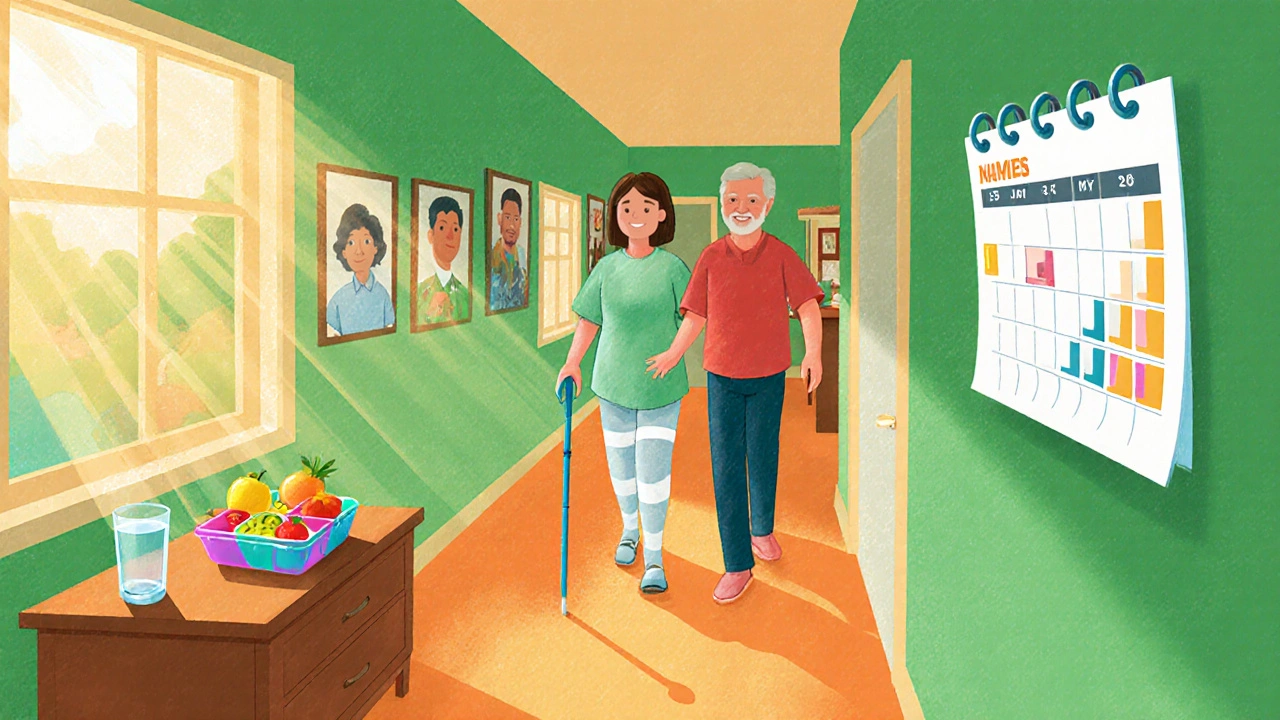
Living with Pulmonary Embolism - Home Care Tips
Recovery isn’t just about taking pills. Here are practical steps families can take:
- Medication adherence: Use a pill organizer or digital reminder. Missing doses can let a clot grow.
- Gradual activity: Start with short walks, avoid long periods of sitting. Compression stockings can help prevent new leg clots.
- Watch for warning signs: New or worsening shortness of breath, chest pain, or swelling in the legs warrants immediate medical attention.
- Diet & hydration: Stay hydrated, especially when on anticoagulants, to reduce bleed risk. Some DOACs advise avoiding high‑fat meals around dosing.
- Follow‑up appointments: Usually a repeat ultrasound or CT at 3‑6 months to ensure the clot is resolving.
Emotional support matters, too. Many patients feel anxious about recurrence. Open conversations, counseling, or support groups can ease that burden.
Preventing Future Episodes
Prevention blends medical and lifestyle measures:
- Identify high‑risk periods: Surgery, prolonged travel, or recovery from injury are key times to discuss prophylaxis with your doctor.
- Pharmacologic prophylaxis: Low‑dose heparin or DOACs may be prescribed for a few weeks after major procedures.
- Mechanical methods: Intermittent pneumatic compression devices during hospital stays reduce DVT risk.
- Lifestyle tweaks: Stay active, maintain a healthy weight, and quit smoking - all lower clot‑forming potential.
- Screen for inherited disorders: If you have a family history of early clotting events, ask about genetic testing for Factor V Leiden or prothrombin gene mutation.
By combining these steps, many people can live clot‑free lives after an initial PE episode.
Frequently Asked Questions
Can a pulmonary embolism resolve on its own?
Small clots can sometimes dissolve naturally, but without anticoagulation the risk of growth or new clots remains high. Medical treatment dramatically improves outcomes.
How long do I need to stay on blood thinners?
Typical treatment lasts 3-6 months for a first‑time, provoked PE. If the clot was unprovoked or you have ongoing risk factors, indefinite therapy may be recommended.
What activities should I avoid during recovery?
Avoid long, uninterrupted periods of sitting or lying down. Heavy lifting and high‑intensity sports should be postponed until your doctor confirms clot stability, usually after several weeks.
Is surgery ever needed for a pulmonary embolism?
Surgery is rare and reserved for massive PE causing heart failure that doesn’t respond to medication. Most cases are managed with anticoagulants alone.
Can COVID‑19 increase my risk of PE?
Yes. The virus can trigger inflammation and clotting abnormalities, making PE more common during and after infection. Hospitalized COVID‑19 patients often receive prophylactic anticoagulation.
Understanding pulmonary embolism empowers you to act fast, follow the right treatment plan, and reduce the chance of another clot. Keep this guide handy, talk openly with your healthcare team, and remember that early detection and proper care make a huge difference.

Harini Prakash
October 22, 2025 AT 20:40Hey there, I’m really glad you found this guide – it’s packed with practical steps that families can actually use without feeling overwhelmed 😊.
First, make sure the patient’s medication schedule is locked in with a pill organizer; missing even one dose can let the clot grow again.
Second, encourage gentle movement as soon as the doctor gives the green light – a short walk around the house or hallway can keep blood flowing and reduce the risk of new clots.
Third, stay hydrated, especially if they’re on anticoagulants, because dehydration can make the blood thicker.
Fourth, watch for any new or worsening shortness of breath, chest pain, or swelling in the legs – these are red flags that need immediate medical attention.
Fifth, if the patient is on a DOAC like apixaban or rivaroxaban, remind them to take it with a light snack and avoid high‑fat meals that might affect absorption.
Sixth, schedule the follow‑up imaging (usually an ultrasound or CT) at the 3‑ to 6‑month mark to confirm the clot is shrinking.
Seventh, consider compression stockings if the doctor recommends them; they help maintain venous return in the legs.
Eighth, keep an open dialogue about anxiety – many survivors feel scared about a recurrence, and talking to a counselor or joining a support group can really help.
Ninth, if the patient has a family history of clotting disorders, ask the doctor about genetic testing for Factor V Leiden or prothrombin mutations.
Tenth, during high‑risk periods like long flights or post‑surgery, discuss prophylactic low‑dose heparin or a short course of a DOAC with the physician.
Eleventh, avoid smoking and maintain a healthy weight; both are modifiable risk factors that make clot formation less likely.
Twelfth, if the patient experiences any unusual bleeding (bruises, blood in urine, or dark stools), contact the healthcare team right away – it could be a sign of over‑anticoagulation.
Thirteenth, educate close friends and family on the signs of PE so they can act fast if something happens when you’re not around.
Fourteenth, keep a written list of all medications, including over‑the‑counter drugs and supplements, because many can interact with blood thinners.
Fifteenth, remember that recovery isn’t linear – some days will feel better than others, and that’s normal.
Sixteenth, celebrate small milestones, like the first week of consistent medication adherence, because every step forward counts. 🙌
Rachael Turner
October 22, 2025 AT 22:30Reading through this, I feel a calm reassurance that knowledge truly empowers us during scary moments.
The way the guide breaks down the Wells score and D‑dimer in plain words makes the medical jargon less intimidating.
It also gently reminds us that even a tiny clot can dissolve on its own, yet treatment is vital to prevent growth.
I appreciate the emphasis on hydration and gradual activity – simple habits that can save lives.
Overall, this feels like a compassionate hand reaching out to families navigating uncertainty.
Kiara Gerardino
October 23, 2025 AT 00:26Honestly, it’s absurd how many people ignore the warning signs until it’s too late.
We need to stop treating pulmonary embolism as a distant myth and start treating it as a real, immediate threat.
The guide rightly calls out prolonged immobility, yet society still glorifies endless flights and sedentary work.
Wake up, educate yourself, and demand prophylaxis when you know you’re at risk.
Tim Blümel
October 23, 2025 AT 01:16That’s a powerful reminder, Kiara.
It’s true that many overlook subtle symptoms, so spreading awareness is key.
One practical tip is to keep a small notebook in the bedside drawer to jot down any sudden breathlessness or chest discomfort – a quick log can help doctors assess the urgency.
Also, asking your surgeon about clot‑prevention measures before a planned operation can make a huge difference.
Let’s keep the conversation going and help each other stay prepared.
Joanne Ponnappa
October 23, 2025 AT 02:40Very useful guide – clear and simple. 👍
Michael Vandiver
October 23, 2025 AT 03:30Glad you think it’s helpful! 😄
My tip: set a daily alarm on your phone to remind you to take the anticoagulant – it’s easy to forget with a busy schedule.
Also, sharing this guide with a friend who’s just out of surgery can give them a head start on prevention.
Emily Collins
October 23, 2025 AT 04:53The emotional toll of a PE is often overlooked; families feel helpless and terrified.
Having a roadmap like this can at least give them a sense of control.
Suryadevan Vasu
October 23, 2025 AT 05:26Stay hydrated and follow the med schedule.
Diane Thurman
October 23, 2025 AT 06:16i cant beleve how many ppl ignore the basic steps like drinking water and packin meds. it's just basic, bbut many still mess up.
Sarah Riley
October 23, 2025 AT 07:06From a pathophysiological standpoint, early activation of the coagulation cascade necessitates prompt pharmacodynamic intervention to mitigate thrombus propagation.
Emma Parker
October 23, 2025 AT 07:56hey diane, i get it sometimes we all forget to breathe deep but this guide is really helpfull
Wade Grindle
October 23, 2025 AT 08:46This guide does a great job of balancing medical detail with everyday language, making it accessible to a wide audience.
Benedict Posadas
October 23, 2025 AT 09:36Totally agree, Wade! 🌟
Let’s keep sharing resources like this – the more people who know, the fewer surprises down the road. 😊