Inflammation: Understanding the Body’s Alarm System
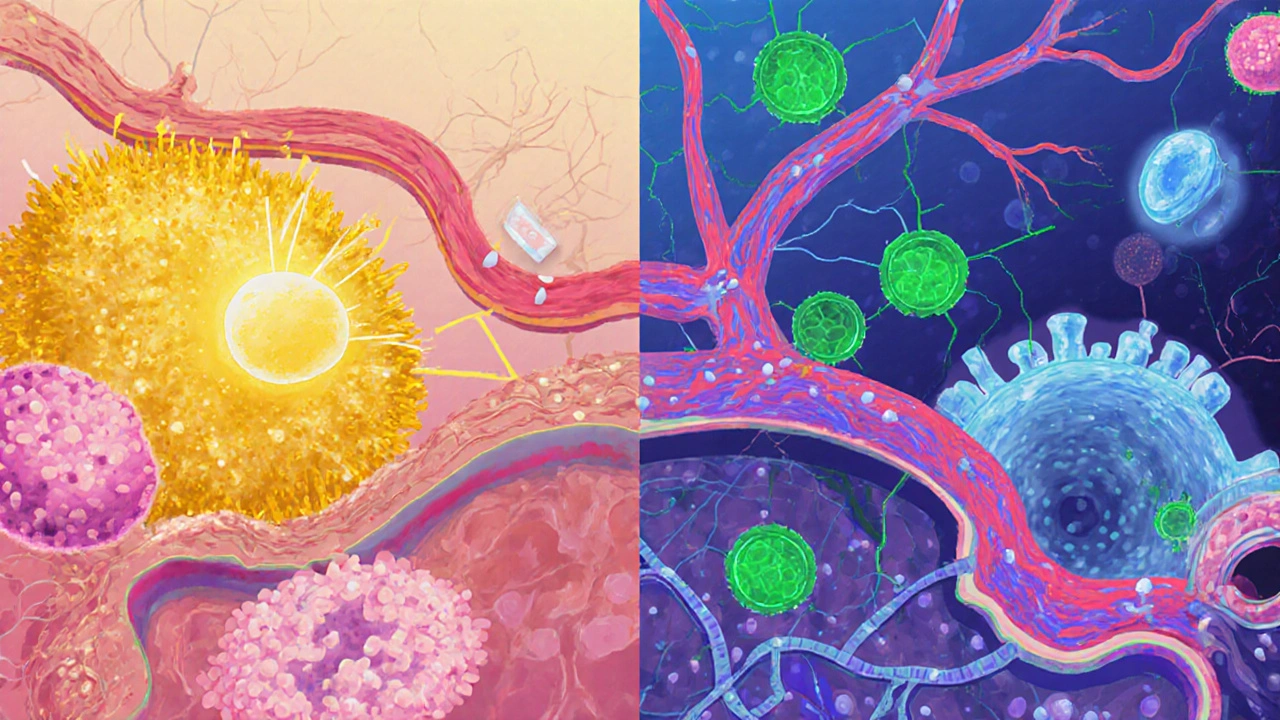
When dealing with Inflammation, the body’s natural response to injury, infection, or irritation that shows up as swelling, heat, redness, and pain. Also known as inflammatory response, it signals that your immune system is on alert. In simple terms, inflammation is the alarm system that tells you something is wrong inside. It can be acute, like the sting from a cut, or chronic, lingering for months and contributing to diseases such as arthritis or heart disease. Inflammation therefore isn’t always the enemy; it’s a protective process that can become harmful when it sticks around too long. One of the most common ways to calm that alarm is through NSAIDs, drugs that block cyclooxygenase enzymes to reduce prostaglandin‑mediated swelling and pain. Ibuprofen, naproxen, and the prescription Celecoxib all fall into this group. Another powerful class is corticosteroids, synthetic hormones that suppress multiple inflammatory pathways, often used for severe flare‑ups such as prednisone or the nasal spray Nasonex. Both NSAIDs and corticosteroids illustrate the semantic triple: Inflammation requires treatment options like NSAIDs and corticosteroids. Beyond pharmaceuticals, many people turn to supplements, natural compounds such as turmeric, omega‑3 fatty acids, or specialized blends like the Purim supplement to modulate the inflammatory cascade. Research shows curcumin can lower certain inflammatory markers, while omega‑3s may help keep chronic low‑grade inflammation in check. This creates another triple: Supplements influence the intensity of inflammation. Triggers range from bacterial infections, like a sinus infection that may need antibiotics, to mechanical stress on joints. When inflammation becomes chronic, it can drive conditions like rheumatoid arthritis, inflammatory bowel disease, or even accelerate atherosclerosis. That’s why doctors often run blood tests for C‑reactive protein (CRP) or erythrocyte sedimentation rate (ESR) to gauge the level of systemic inflammation. Knowing the level helps decide if you stay with over‑the‑counter NSAIDs, step up to prescription options, or add a corticosteroid burst. Each option carries trade‑offs: NSAIDs may irritate the stomach lining, corticosteroids can raise blood sugar, and supplements might interact with meds.
Key Ways to Tame Inflammation
When inflammation is driven by an infection, doctors frequently prescribe antibiotics, medicines that kill or inhibit bacteria and can reduce infection‑related swelling. Choosing the right antibiotic matters; for example, Vantin (cefpodoxime) may be preferred over amoxicillin for certain urinary tract infections, while Omnicef (cefdinir) offers a broader spectrum for respiratory bugs. Levofloxacin provides high tissue penetration but carries a higher risk of tendon issues, so it’s reserved for tougher cases. Understanding these nuances helps you match the drug to the cause of inflammation without over‑using broad‑spectrum agents. Because many of these medicines are available as cheap generics, knowing how to buy them safely online can save you a lot of money. Guides on purchasing generic Tamoxifen, Celecoxib, Metformin, and even specialty items like the I‑Pill teach you how to verify pharmacy credentials, compare prices, and avoid counterfeit products. The same principles apply to antibiotics and anti‑inflammatory drugs: look for a licensed pharmacy, check that a prescription is required, and read user reviews for reliability. By applying a consistent safety checklist, you reduce the risk of harmful side effects and ensure you get the intended therapeutic effect. All the articles below walk you through these steps with real‑world examples, price comparisons, and safety tips. Whether you’re managing a flare‑up, hunting for a cost‑effective generic, or simply curious about how different drug classes handle inflammation, the collection provides practical insight you can act on right away.
Below you’ll find a curated set of guides that break down buying cheap generics, comparing drug efficacy, and spotting safety red flags for the medications that target inflammation.
- 17 Comments
Explore how allergic disorders and autoimmune diseases share genetic, environmental, and inflammatory pathways, and learn practical steps to manage both conditions.
