Drug Manufacturing: How Generic Medicines Are Made and Regulated
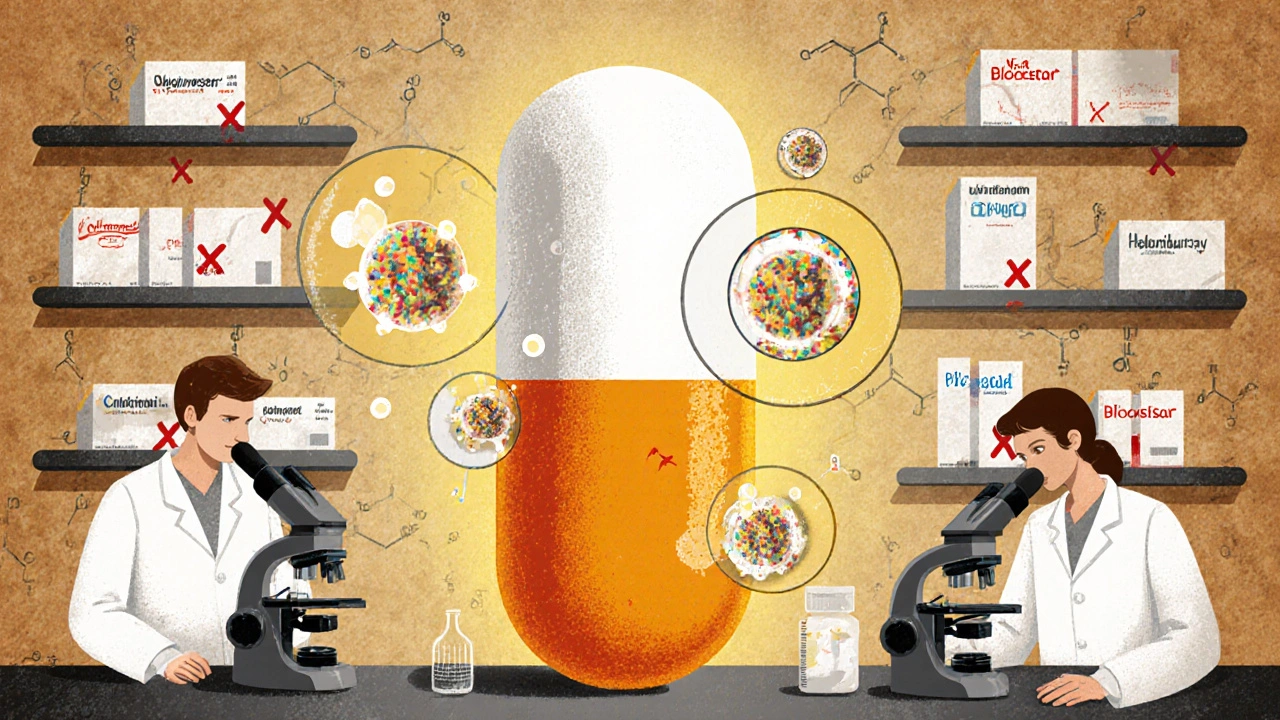
When you pick up a generic pill at the pharmacy, you might think it’s just a cheaper copy—but drug manufacturing, the process of producing medications under strict scientific and regulatory standards. Also known as pharmaceutical production, it’s a complex chain that starts in labs and ends in your medicine cabinet. This isn’t guesswork. Every batch of generic drug must meet the same purity, strength, and performance standards as the brand-name version. The FDA doesn’t just approve the idea—it demands proof, through tests like in vivo bioequivalence, human trials that measure how the body absorbs the drug and in vitro dissolution, lab tests that check how the pill breaks down under controlled conditions. If the numbers don’t match, the drug gets rejected.
Behind every approved generic is a document called an ANDA, an Abbreviated New Drug Application that proves the generic is therapeutically equivalent to the brand. This isn’t a shortcut—it’s a rigorous process. Manufacturers must show their product performs the same way under real-world conditions: same absorption rate, same shelf life, same stability under heat and humidity. That’s why stability testing, the process of tracking how a drug changes over time under different storage conditions is so critical. A pill that works today might break down in six months if the manufacturing process isn’t precise. And it’s not just about the active ingredient. The fillers, coatings, and even the color matter. The FDA checks every component to make sure nothing interferes with safety or effectiveness.
But drug manufacturing doesn’t stop at mass-produced pills. Sometimes, standard drugs don’t work for a patient—maybe they’re allergic to a dye, or need a different dose, or can’t swallow pills. That’s where pharmaceutical compounding, the custom mixing of medications to meet individual patient needs comes in. It’s not a loophole—it’s a lifeline. But it’s also less regulated than factory-made drugs. That’s why knowing the difference between FDA-approved generics and compounded prescriptions matters. One is tested across thousands of batches. The other is made one at a time, often without the same level of oversight.
What you’ll find below is a collection of real, practical guides that pull back the curtain on how drugs get made, approved, and delivered. From how the FDA catches unsafe batches to why some generics get delayed, from the science behind bioequivalence to the hidden risks in unregulated supply chains—you’ll see how the system works, where it breaks, and what you can do to stay safe. No fluff. No jargon. Just what you need to understand the medicines you take.
- 11 Comments
Generic drugs save billions in healthcare costs and make up 90% of U.S. prescriptions. Learn how they're made, from reverse-engineering brand-name pills to FDA-approved manufacturing under strict quality controls.
