When you’ve had a severe reaction to a drug, it’s natural to want to avoid anything even remotely similar. But not all drug reactions mean you need to avoid an entire family of medications. In fact, over-avoidance can be just as dangerous as under-avoidance. The key is understanding the type of reaction you had, not just the name of the drug.
Not All Drug Reactions Are Allergies
Many people think a rash or stomach upset means they’re "allergic" to a drug. But most severe reactions-up to 90%-aren’t allergic at all. True drug allergies involve your immune system. Symptoms like hives, swelling of the lips or throat, trouble breathing, or anaphylaxis usually show up within minutes to a few hours after taking the drug. These are the reactions that demand serious caution. On the other hand, side effects like nausea, dizziness, or a mild skin rash are often just predictable side effects of how the drug works in your body. For example, amoxicillin causes a non-allergic rash in 5-10% of people, especially those with mononucleosis. That doesn’t mean you’re allergic to all penicillins. Avoiding the whole family based on this alone can leave you with fewer treatment options when you really need them.When Avoiding the Whole Family Is Necessary
There are a few severe reactions where avoiding the entire medication class is almost always required. These include:- Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) - These are life-threatening skin conditions where large areas of skin detach. TEN has a mortality rate of 30-50%. If you’ve had either, you must permanently avoid the entire drug class that caused it. Common culprits include sulfa antibiotics, anticonvulsants like carbamazepine, and allopurinol.
- DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) - This reaction affects multiple organs and can cause long-term damage to the liver, kidneys, or lungs. Once you’ve had DRESS from a drug, you should never take another drug in that class.
- Anaphylaxis - A full-body allergic reaction that can shut down breathing and blood pressure. If you’ve had this, avoiding the entire drug family is standard until proven otherwise through testing.
The European Medicines Agency found that 95% of TEN cases are caused by just six drug classes. If your reaction was one of these, the rule is simple: don’t take anything in that class again.
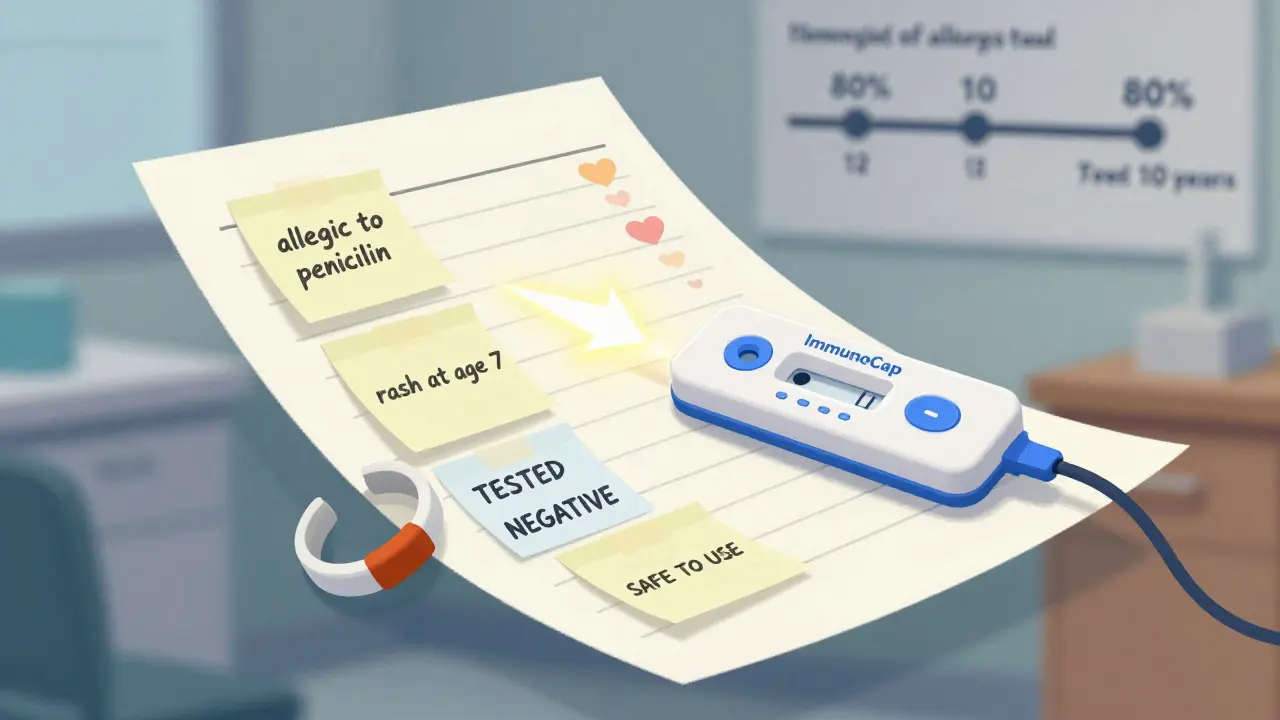
Penicillin Allergy: The Most Common Mislabel
About 10% of people say they’re allergic to penicillin. But studies show that 95% of those people can actually take penicillin safely after proper testing. Many were labeled allergic after a mild rash as a child, or because a family member had a reaction. Over time, true allergies often fade. The American College of Allergy, Asthma, and Immunology found that only 10% of people with a penicillin label have a true IgE-mediated allergy. Skin testing and oral challenges under medical supervision can confirm this. A 2023 study in JAMA Internal Medicine showed that when patients were properly tested, 92% of them could safely take penicillin or related antibiotics like amoxicillin. Avoiding penicillin unnecessarily means doctors use broader-spectrum drugs, which can lead to more side effects and antibiotic resistance.
Other High-Risk Drug Families
Some drug classes have high cross-reactivity rates. If you’ve had a severe reaction to one, you likely need to avoid others in the same group:- Sulfa antibiotics - Drugs like Bactrim and Septra. Cross-reactivity with other sulfa-containing drugs (like some diabetes or diuretic pills) is around 10%. But not all sulfa drugs are the same. A reaction to Bactrim doesn’t automatically mean you can’t take furosemide (Lasix) or sulfonylureas (glipizide), but most doctors err on the side of caution.
- NSAIDs - Aspirin, ibuprofen, naproxen. For most people, switching from one NSAID to another is fine. But if you have aspirin-exacerbated respiratory disease (AERD), you’ll likely react to all traditional NSAIDs. About 70% of people with this condition can’t tolerate any of them. COX-2 inhibitors like celecoxib may be safer options.
- Beta-lactam antibiotics - Penicillins, cephalosporins, carbapenems. Cross-reactivity between penicillins and cephalosporins is low-only 0.5-6.5% depending on the specific drugs. Newer cephalosporins like cefdinir have even lower risk. But if you had anaphylaxis to penicillin, testing before using cephalosporins is recommended.
What to Do After a Severe Reaction
If you’ve had a severe reaction, don’t just accept the label. Follow these steps:- Document the reaction in detail - What drug? When did symptoms start? What were they? Did you need epinephrine or hospitalization? Write it down. Vague notes like "allergic to penicillin" are useless.
- Ask for a referral - Talk to your doctor about seeing an allergist. They can perform skin tests or drug challenges to confirm whether you’re truly allergic.
- Get tested - The FDA-approved ImmunoCap Specific IgE test now has 89% accuracy for drug allergies. Genetic testing for HLA-B*57:01 can safely rule out abacavir reactions in HIV patients.
- Update your records - Make sure your EHR, pharmacy, and emergency card reflect the correct diagnosis. A 2021 study found only 28% of allergy entries in electronic health records had enough detail to guide safe prescribing.
- Consider medical alert jewelry - If you truly have a life-threatening allergy, wear a medical ID bracelet. 78% of allergists recommend this for patients with anaphylaxis.
Why Over-Avoidance Hurts
Avoiding entire drug classes without proof can have real consequences. A survey by the Asthma and Allergy Foundation of America found that 42% of patients with drug allergy labels experienced treatment delays-on average, 3.2 days longer than needed. In one case, a patient with a UTI was denied antibiotics for days because doctors refused all sulfa drugs after a past reaction, even though the reaction wasn’t an allergy. Doctors end up prescribing broader-spectrum antibiotics, which are more expensive, more likely to cause side effects like C. diff infection, and contribute to antibiotic resistance. The NIH’s Preventing Overrides of Severe Drug Allergy Alerts Initiative showed that better documentation and testing reduced inappropriate overrides of allergy alerts by 37%.Future of Drug Allergy Management
New tools are making it easier to get answers. AI systems like IBM Watson for Drug Safety have cut inappropriate avoidance recommendations by 41% in clinical trials. The FDA’s Safer Technologies Program is funding new diagnostic devices. And the All of Us Research Program has identified genetic markers that predict hypersensitivity with near-perfect accuracy. The goal isn’t to avoid drugs. It’s to avoid unnecessary avoidance. With better testing and clearer guidelines, we’re moving toward a future where patients get the right drug-not just the safest one.If I had a rash from one antibiotic, do I need to avoid all antibiotics?
No. Most rashes from antibiotics like amoxicillin are not allergic-they’re side effects. Only if the rash was accompanied by swelling, breathing trouble, or blistering should you avoid the entire class. A mild, flat, non-itchy rash that appeared after several days is unlikely to be a true allergy. See an allergist for testing before assuming you’re allergic to all antibiotics.
Can I ever take a drug I was allergic to again?
Yes, in some cases. If your reaction was mild (like a rash without breathing issues) and occurred years ago, your allergy may have faded. Drug challenges under medical supervision-where you take small, increasing doses of the drug-are safe and successful in 70-85% of cases, especially for penicillins. This is not something to try at home. Always do it with an allergist present.
Is a sulfa allergy the same as a sulfite allergy?
No. Sulfa drugs (like Bactrim) contain a chemical called sulfonamide. Sulfites are preservatives found in wine, dried fruit, and some medications. A reaction to sulfites (like wheezing after wine) does not mean you’re allergic to sulfa antibiotics. They’re completely different chemicals. If you’re allergic to sulfites, you can still take sulfa drugs, and vice versa.
Why do some doctors refuse to prescribe any drug from a class after one reaction?
Many doctors aren’t trained in allergy specifics. They see "penicillin allergy" in the chart and assume the whole class is off-limits. This is outdated thinking. Guidelines from the American Academy of Allergy and the FDA now say that unless the reaction was life-threatening or immune-mediated, cross-reactivity risk is low. But without clear documentation, doctors play it safe-and that can hurt patients.
Can I outgrow a drug allergy?
Yes. Drug allergies, especially IgE-mediated ones like penicillin, can fade over time. Studies show that 50% of people lose their allergy within five years, and 80% lose it after ten years. That’s why retesting is so important. If you were labeled allergic as a child, it’s very likely you can now safely take the drug.

