Every time you pick up a prescription, you’re handed a small piece of paper or a sticker with a lot of writing on it. It might look like gibberish. But every line, number, and word on that label is there for a reason - and understanding it could keep you safe. You don’t need to be a doctor to read it. You just need to know what each part means.
Your Name Is There for a Reason
At the top of every prescription label, you’ll see your full name. It seems obvious, but this isn’t just for record-keeping. It’s a safety guard. In the U.S., about 1.5 million medication errors happen every year, and many of them are caused by mixing up patients. One wrong pill given to the wrong person can lead to serious harm. Your name on the label ensures the pharmacist double-checks they’re giving your medicine - not someone else’s. If your name isn’t there, don’t take it. Ask for clarification.
The Medication Name: Brand vs. Generic
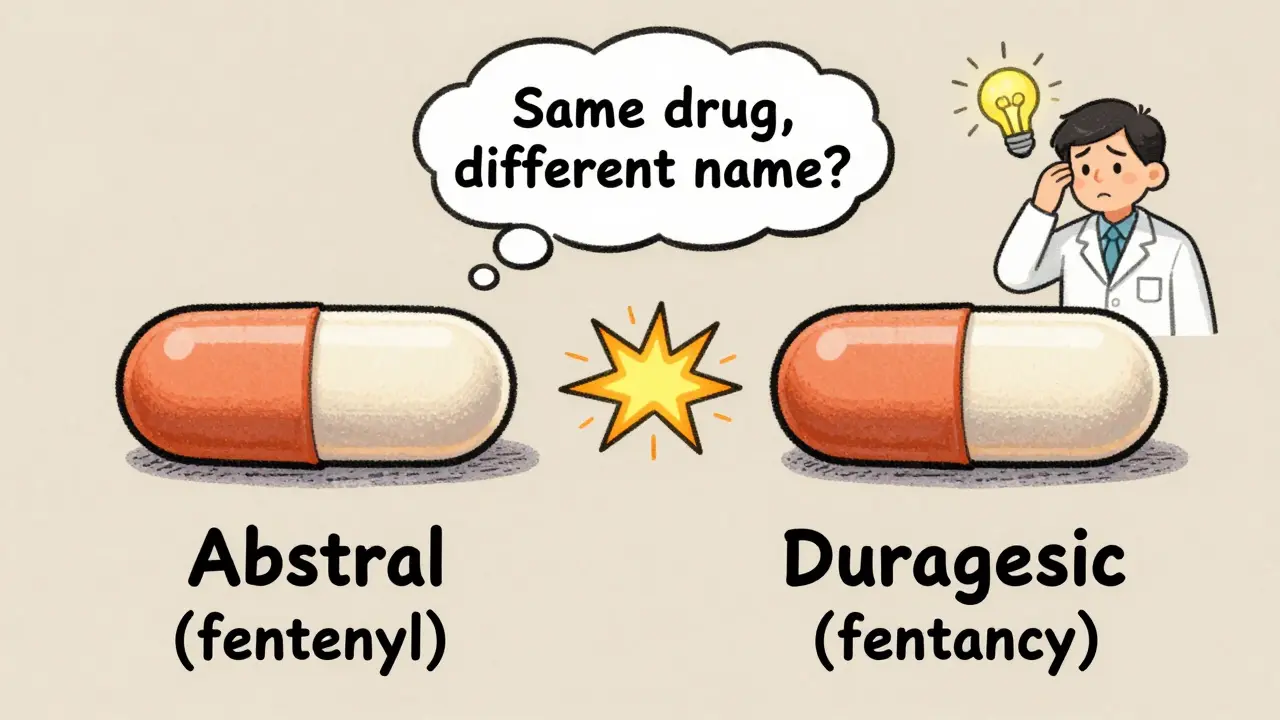
You’ll see two names for your drug. The first is the brand name - like Abstral. The second is the generic name - fentanyl. The brand name is what the company calls it when they sell it. The generic name is the actual chemical in the pill. Knowing the generic name helps you avoid duplicates. For example, if your doctor prescribes fentanyl and your pharmacist gives you Abstral, you’re getting the same thing. But if you’re also taking another painkiller called Duragesic (which is also fentanyl), you could accidentally double your dose. Always check the generic name. It’s your best tool to avoid taking the same drug twice.
Dosage Strength: How Much Is in Each Pill?
Look for numbers like “100 mcg” or “50 mg.” That’s the strength of each pill or dose. It tells you exactly how much active medicine is inside. A 100 mcg fentanyl tablet is much stronger than a 25 mcg one. If you’re confused, ask: “Is this the same strength as last time?” Many errors happen because patients assume all pills of the same drug are equal. They’re not. A 2021 study from the Institute for Safe Medication Practices found that 37% of patients misread dosage numbers, especially when written in small font. Always confirm the number matches what your doctor told you.
How and When to Take It
This part tells you how often to take the medicine and under what conditions. It might say: “Take one tablet by mouth every 4 hours as needed for pain.” Or: “Take with food, once daily in the morning.” Pay attention to words like “as needed,” “daily,” or “before meals.” If it says “take with food,” skipping that can make the drug less effective - or even cause stomach upset. If it says “take on an empty stomach,” eating too soon can block absorption. And watch out for abbreviations. “QD” means once daily. “BID” means twice a day. But many pharmacies now spell these out because abbreviations like “QD” have been mistaken for “QID” (four times a day), leading to dangerous overdoses. If you see an abbreviation you don’t understand, ask.
Expiration Date: When It Stops Working
The expiration date isn’t just a suggestion. It’s the last day the manufacturer guarantees the drug is fully potent and safe. Most prescriptions expire 12 to 18 months after being filled. After that, the medicine might not work as well - or could break down into harmful substances. The FDA doesn’t require expiration dates on all prescriptions, but most pharmacies follow U.S. Pharmacopeia standards. Don’t take medicine past its expiration date. Especially antibiotics, insulin, or heart medications. A 2022 study showed that 41% of people kept expired pills, and 17% took them anyway. That’s risky.
The Rx Number: Your Prescription’s ID
This number - usually starting with “Rx” - is your prescription’s unique code. It’s how the pharmacy tracks your refill history. If you call for a refill, they’ll ask for this number. If you switch pharmacies, they’ll need it to transfer your record. But it’s not just for logistics. If you have a problem - like a bad reaction - the Rx number helps the pharmacy trace exactly which batch of medicine you got. That’s critical if there’s a recall. Always keep this number handy.
Pharmacy and Prescriber Info: Who to Call
Look for the pharmacy’s name, phone number, and address. Also, you’ll see your doctor’s name. These aren’t just for show. If you have a question - like “Why am I taking this?” or “Is this safe with my other meds?” - call the pharmacy. Pharmacists are trained to answer these questions. They can check for dangerous interactions. They can explain side effects. You don’t need to wait for an appointment. In fact, a 2021 JAMA Internal Medicine study found that patients who talked to their pharmacist after getting a new prescription were 28% more likely to take it correctly. And if you notice a mistake - like the wrong drug or dose - call the pharmacy immediately. They can fix it before you take it.
What the Pill Looks Like: Color, Shape, Imprint
Some labels include a description: “white, round, scored tablet” or “blue, capsule, imprinted with A123.” This helps you confirm you got the right pill, especially if you refill at a different pharmacy. Pills from different manufacturers can look different, even if they’re the same drug. If your pill suddenly looks different, don’t assume it’s a mistake. But do check. Ask: “Is this the same medicine?” A 2023 survey found that 33% of patients didn’t recognize a change in pill appearance - and took the wrong drug because of it.
The NDC Number: The Drug’s Official ID
You’ll see a 10- or 11-digit number - the National Drug Code (NDC). It’s not meant for you to memorize, but it’s important. This code tells the pharmacy system exactly which drug, strength, and package size you received. It’s used for billing, tracking recalls, and insurance claims. If there’s ever a recall, the NDC helps identify your batch. You can look it up online if you’re curious, but you don’t need to. Just know it’s there to ensure accuracy.

Storage Instructions: Keep It Safe
Some labels say: “Store at room temperature” or “Refrigerate.” Others say: “Keep away from moisture.” These aren’t optional. Heat, humidity, or light can break down medicine. Insulin, for example, loses its power if left out too long. Antibiotics can become ineffective. If your label says “refrigerate,” keep it in the fridge - not on the counter. If it says “protect from light,” keep it in its original container. A 2022 FDA report found that 29% of patients stored medications incorrectly, leading to reduced effectiveness. Don’t guess. Follow the label.
Warnings: The Red Flags
This section might say: “May cause drowsiness,” “Avoid alcohol,” or “Not for use in pregnancy.” These are serious. They’re based on real risks. A 2023 FDA review found that 68% of hospital admissions from medication errors involved drugs with clear warnings that patients ignored. If your label says “Do not drive,” don’t. If it says “Avoid grapefruit,” skip the fruit. These aren’t suggestions. They’re safety rules. If you’re unsure why a warning exists, ask your pharmacist. They can explain the science behind it.
The Most Important Missing Piece: Why You’re Taking It
Here’s the big one: most labels still don’t say why you’re taking the medicine. Is it for high blood pressure? Depression? Infection? That’s a gap. The FDA recommends including the reason - and studies show it cuts errors. A 2022 study from the Institute for Safe Medication Practices found that when the indication was added to labels, wrong-drug errors dropped by 55%. Imagine taking a pill for blood pressure when you actually need it for anxiety. That’s dangerous. Some pharmacies now add this - like “For high cholesterol” or “For thyroid condition.” If yours doesn’t, ask. Say: “Can you write down why I’m taking this?” It’s your right. And by 2025, the U.S. Pharmacopeia expects all prescriptions to include this.
What to Do When You’re Confused
Don’t guess. Don’t assume. Don’t look it up online without checking with a professional. Use the FDA’s five questions:
- What is the name of the medication and what is it for?
- How and when do I take it?
- What should I do if I miss a dose?
- What side effects should I expect?
- Will this interact with other drugs I take?
Also, try the “Ask Me 3” method: 1) What is my main problem? 2) What do I need to do? 3) Why is it important? If you can’t answer these after reading the label, call your pharmacist. They’re trained to help. And if they don’t explain clearly, ask again. You’re not being difficult - you’re being smart.
Final Tip: Check Every Time
Even if you’ve taken the same medicine for years, check the label every refill. Pills change. Doses change. Pharmacies change. A 2023 Cleveland Clinic study found that 22% of long-term patients received the wrong dose on a refill - and didn’t notice until they had side effects. Always compare the new label to the old one. Look for changes in name, number, color, or instructions. If anything’s different, pause. Ask. It could save your life.


Taylor Mead
February 17, 2026 AT 14:51