Medication Timing Calculator
Medication Timing Assistant
Enter your medications to learn optimal timing, risks, and side effects based on chronotherapy research
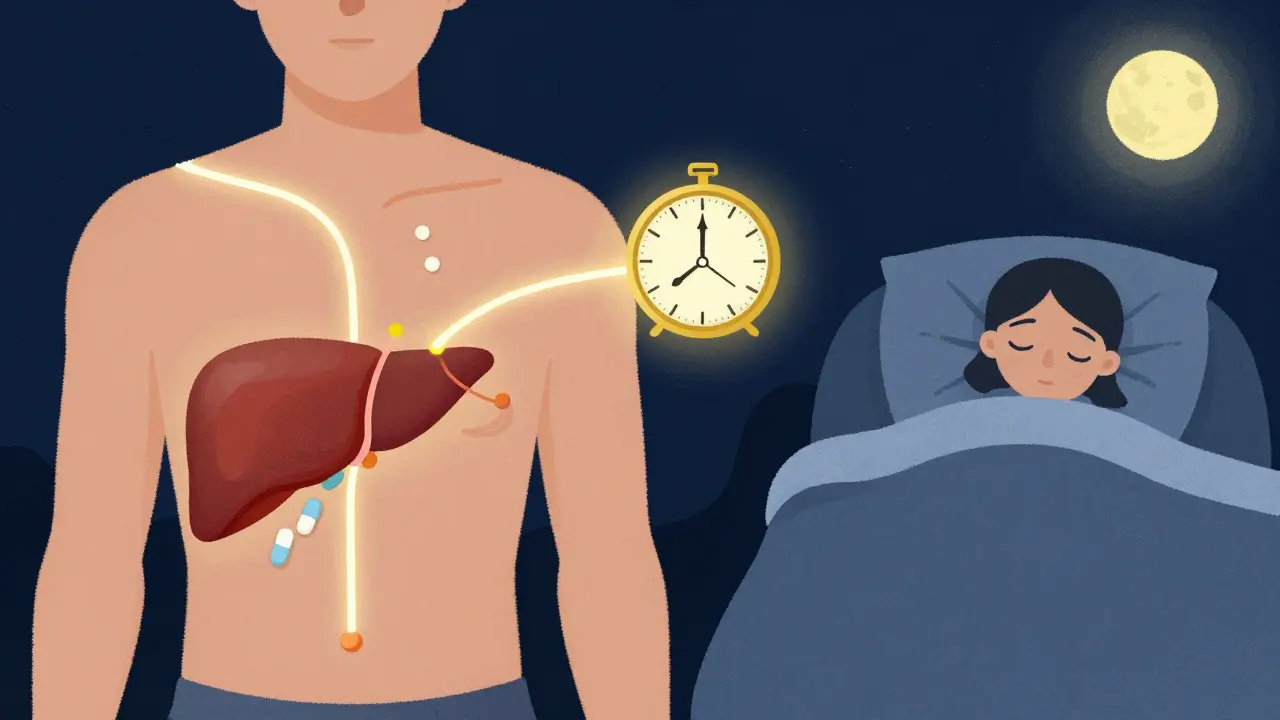
Have you ever wondered why your doctor told you to take your blood pressure pill at night, or your statin before bed? It’s not just a random rule. The time you take your medication can make a real difference in how well it works-and how many side effects you feel. This isn’t guesswork. It’s science. And it’s called chronotherapy.
Why Timing Matters More Than You Think
Your body runs on a 24-hour clock. Not just your sleep cycle, but your liver, kidneys, heart, and even your stomach lining follow daily rhythms. These rhythms affect how your body absorbs, processes, and gets rid of drugs. Take the same pill at 8 a.m. versus 8 p.m., and your body might handle it completely differently. For example, cholesterol production peaks at night. That’s why statins like atorvastatin and simvastatin work better when taken in the evening. Studies show they lower LDL (bad) cholesterol by 15-20% more than when taken in the morning. It’s not about the dose. It’s about the timing. Same goes for blood pressure meds. A major study called MAPEC found that taking ACE inhibitors at bedtime cut cardiovascular events-like heart attacks and strokes-by 29% compared to morning dosing. Why? Because blood pressure naturally dips at night, and hitting that window with the right drug helps keep it stable.When Timing Goes Wrong: The Real Cost of Mistakes
Getting the time wrong isn’t just inconvenient-it can be dangerous. Some drugs have razor-thin windows for safe use. Insulin is one of them. If you take your rapid-acting insulin 30 minutes too early before a meal, your blood sugar can crash. Research shows mistimed insulin causes hypoglycemia in 22% of cases. That’s not rare. That’s common. Anticoagulants like warfarin or rivaroxaban are another example. Even a few hours off schedule can raise your bleeding risk by up to 37%. A single missed dose or delayed dose doesn’t just mean “I’ll take it later.” It means your blood’s clotting ability is out of balance. And then there’s chemotherapy. In oncology, timing isn’t just about comfort-it’s about survival. Deviating from the scheduled window by more than 30 minutes can reduce treatment effectiveness by 15-20%. That’s not a small drop. That’s the difference between beating cancer and watching it come back.Not All Medicines Are Created Equal
Here’s the thing: not every drug needs perfect timing. Some are forgiving. Others aren’t.- High-risk, timing-critical: Insulin, anticoagulants, chemotherapy, certain pain meds like morphine (must be given within 10-15 minutes of scheduled time), and some seizure drugs.
- Medium-risk: Beta-blockers, thyroid meds, corticosteroids (like prednisone), and some diuretics. A 1-2 hour window is usually okay, but consistency matters.
- Low-risk: Most statins (evening is best, but morning won’t ruin it), many antibiotics, and routine supplements like calcium or vitamin D.

Why Hospitals Struggle (And So Do Homes)
In hospitals, nurses are often interrupted 5 or more times during a single med pass. Studies show that with 5 interruptions, medication errors jump from 39% to 61%. That’s more than double. Timing gets lost in the shuffle. And it’s not just hospitals. At home, 68% of people taking chronotherapy-recommended meds-like evening statins or bedtime blood pressure pills-don’t stick to the schedule. Why? Work shifts, forgetfulness, travel, or just not understanding why it matters. One patient told researchers, “I take it when I remember.” That’s not enough. Caregivers face the same problem. A survey found that 52% of timing errors happened because work schedules clashed with medication times. If you work nights, taking a pill at 7 p.m. isn’t an option. But skipping it or taking it at 3 a.m. might be worse.How Technology Is Helping
Electronic health records are starting to catch up. Epic Systems released a module called ChronoCare in 2023 that flags high-risk medications and suggests optimal timing windows based on your sleep schedule. It doesn’t just say “take at bedtime.” It asks: “Do you go to sleep at 11 p.m. or 2 a.m.? Let’s adjust.” Barcode systems in hospitals have cut timing errors by 28%. Why? Because they force a check: Is this the right drug? Right patient? Right time? No more guessing. Even your phone can help. Apps that sync with your pharmacy and send alerts based on your personal rhythm are becoming more common. Some even learn your habits and nudge you if you’re running late.
What You Can Do Right Now
You don’t need a PhD to get this right. Here’s what actually works:- Ask your pharmacist. Not your doctor. Pharmacists know the timing rules inside and out. Ask: “Which of my meds need strict timing?”
- Use a pill organizer with alarms. Not just a box. One with a timer that beeps. Set it for the exact time your med needs to be taken.
- Link meds to habits. Take your evening pill after brushing your teeth. Take your morning pill with breakfast. Habit stacking makes it stick.
- Track your side effects. Keep a simple log: “Took at 7 p.m. → no dizziness. Took at 11 p.m. → felt foggy.” Patterns tell you what works.
- Speak up if your schedule changes. Working nights? Traveling? Going on vacation? Call your pharmacy. Timing might need to shift.
The Bigger Picture
The global chronotherapy market is growing fast-projected to hit $32.4 billion by 2027. Why? Because the evidence is piling up. The FDA now requires chronopharmacology data for 17 new drugs each year. That’s up from just 3 in 2018. This isn’t fringe science. It’s becoming standard. And it’s not about making life harder. It’s about making treatment safer, more effective, and less painful. The next time you’re told to take a pill at a certain time, don’t just nod and move on. Ask why. The answer might just change your health.Can I take my medication at a different time if I forget?
It depends on the drug. For high-risk meds like insulin, anticoagulants, or chemotherapy, never skip or delay without checking your provider. For others, like statins or blood pressure pills, taking it up to 2 hours late is usually okay-but don’t make it a habit. Consistency matters more than perfection.
Why do some drugs work better at night?
Your body’s internal clock controls how fast your liver breaks down drugs, how well your kidneys filter them, and even how your stomach absorbs them. For example, cholesterol production peaks between midnight and 4 a.m., so statins taken at night block more of it. Blood pressure naturally dips at night, so taking ACE inhibitors then helps maintain that dip, reducing strain on your heart.
Are there side effects from taking meds at the wrong time?
Yes. Taking blood pressure meds in the morning instead of at night can lead to uncontrolled highs during sleep, increasing stroke risk. Taking insulin too early can cause dangerous lows. Even something as simple as a steroid like prednisone taken at night can cause insomnia. Timing affects both effectiveness and side effects.
Do I need to take all my meds at the exact same time every day?
No. Only the high-risk ones require strict timing. Most antibiotics, supplements, and pain relievers have a flexible window. But for insulin, anticoagulants, chemotherapy, and some heart meds, being off by even an hour can matter. Always ask your pharmacist which ones need precision.
Can my sleep schedule affect how my meds work?
Absolutely. If you work night shifts or have irregular sleep, your body’s internal clock shifts. That changes how drugs are processed. A night-shift worker taking a morning pill might get more side effects because their liver isn’t ready. Talk to your provider if your schedule changes-it might mean adjusting your dosing time.

Gloria Ricky
February 11, 2026 AT 00:18Vamsi Krishna
February 11, 2026 AT 17:10Brad Ralph
February 12, 2026 AT 00:02Suzette Smith
February 13, 2026 AT 10:14Autumn Frankart
February 14, 2026 AT 05:46Stephon Devereux
February 16, 2026 AT 02:27steve sunio
February 16, 2026 AT 19:37athmaja biju
February 17, 2026 AT 21:44