What’s the difference between a TIA and a stroke?
You wake up one morning and your arm feels numb. Your speech is slurred. You’re dizzy. Then, just as suddenly, it’s gone. No pain. No lasting damage. You think, It must’ve been nothing. But if you’ve had those symptoms-even for five minutes-you’ve likely had a TIA. And it’s not a warning. It’s a red alert.
A TIA, or transient ischemic attack, is often called a ‘mini-stroke.’ That term is dangerously wrong. It makes people think it’s minor. It’s not. A TIA is your brain screaming for help. It’s a temporary blockage in a blood vessel feeding the brain. The symptoms vanish because the clot breaks up or moves. But that doesn’t mean the danger is over. In fact, it’s just getting started.
A stroke, on the other hand, is when that blockage doesn’t clear. Brain cells die. Permanent damage happens. You might lose movement, speech, or memory. The difference between a TIA and a stroke isn’t how bad the symptoms feel. It’s whether the brain tissue is permanently injured. And here’s the kicker: up to 35% of people who think they had a TIA actually had a minor stroke. Their brain was already damaged, but they didn’t know because the symptoms faded.
The symptoms are the same-so how do you tell them apart?
There’s no secret code. The symptoms of a TIA and an ischemic stroke are identical. That’s why you don’t wait to see if it gets worse. You act immediately.
- Face drooping: One side of the face sags when smiling. Ask the person to smile. Is it uneven?
- Arm weakness: Can they raise both arms? Does one drift downward?
- Speech trouble: Is their speech slurred, strange, or hard to understand? Ask them to repeat a simple sentence like ‘The sky is blue.’
- Vision loss: Sudden blur or blackness in one or both eyes.
- Dizziness or loss of balance: No cause, no spinning, just sudden unsteadiness.
- Severe headache: Comes out of nowhere. No migraine history. Feels like the worst headache of your life.
This is the BE FAST rule: Balance, Eyes, Face, Arm, Speech, Time to call 911. It applies to both TIA and stroke. If you see any of these-even if they go away in 10 minutes-call emergency services. Right now. Don’t wait. Don’t text a friend. Don’t Google it. Call 911.
Why a TIA is more dangerous than it looks
People think, ‘If it’s gone, it’s fine.’ That’s the biggest mistake in stroke prevention.
One in five people who have a TIA will have a full stroke within 90 days. Half of those happen in the first two days. The highest risk? The first 48 hours. That’s when your brain is still vulnerable. The clot that caused the TIA might come back. Or another one forms. Or your arteries are so clogged, another blockage is inevitable.
Studies show that if you get treated within 24 hours of a TIA, your stroke risk drops by 80%. Delay treatment beyond 48 hours, and your risk skyrockets. Yet, 31% of people wait more than 24 hours to get help-even after clear symptoms. Why? Because they think it’s not serious. It’s not. It’s a countdown.
And here’s something most don’t know: up to 48% of people who have a TIA show hidden brain damage on advanced MRI scans. That means even if you feel fine, your brain might already be hurt. A TIA isn’t just a warning. It’s proof your brain has already been under attack.
What happens when you get to the hospital?
Don’t assume you’ll just get a CT scan and go home. A TIA needs a full emergency evaluation.
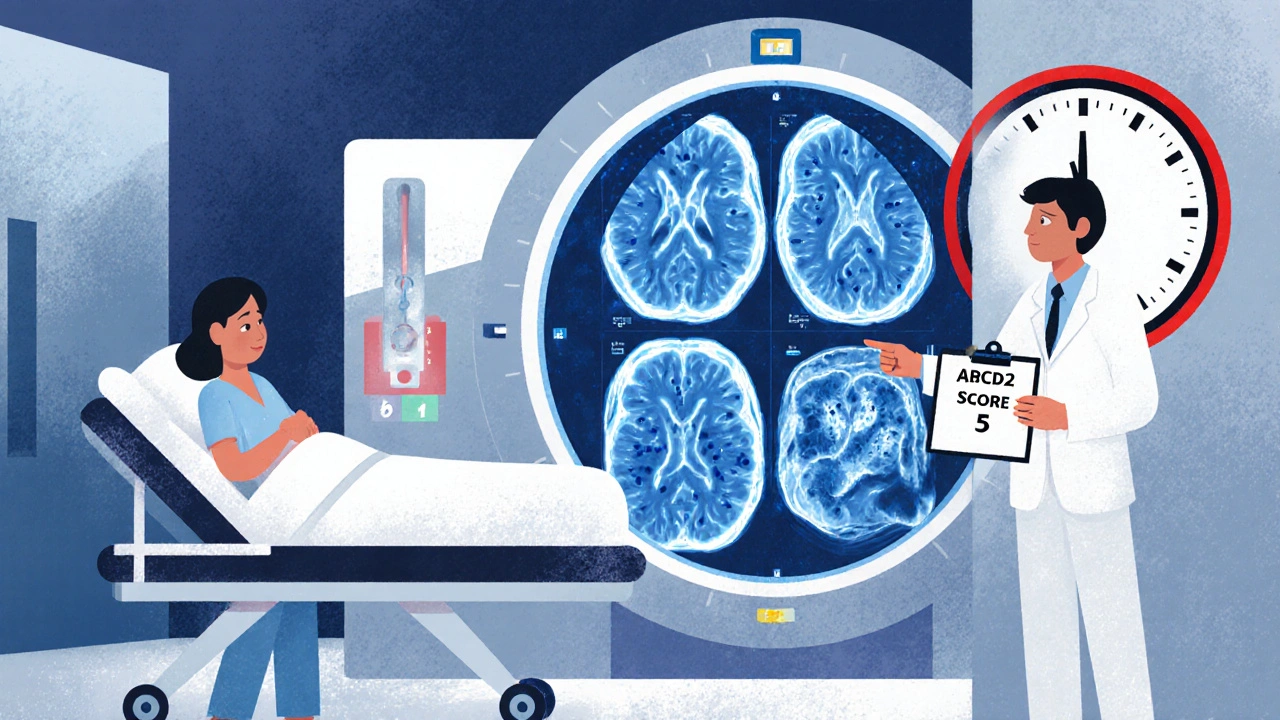
First, they’ll rule out a brain bleed with a non-contrast CT scan. Then, they’ll order an MRI with diffusion-weighted imaging. This is the gold standard. It can detect tiny areas of brain damage that a regular CT misses. If the MRI shows a stroke, your diagnosis changes. You’re not having a TIA-you had a minor stroke. Treatment is the same, but the urgency is even higher.
Doctors use the ABCD2 score to figure out your risk:
- Age: Over 60? +1 point
- Blood pressure: Higher than 140/90? +1 point
- Clinical features: Weakness on one side? +2 points. Just speech trouble? +1 point
- Duration: Symptoms over 60 minutes? +2 points. 10-59 minutes? +1 point
- Diabetes: Do you have it? +1 point
A score of 4 or higher means you’re high risk. You need to be admitted to the hospital-fast. Low risk? Still, you need to be seen within 24 hours. No exceptions.
What’s the treatment after a TIA?
Treatment starts the moment you’re diagnosed. It’s not about fixing the past. It’s about stopping the next stroke.
Within 24 hours, you’ll get:
- Aspirin: 325 mg. Reduces your next stroke risk by 60%.
- Dual antiplatelet therapy: Aspirin + clopidogrel. Given for 21 to 30 days. Lowers stroke risk even more than aspirin alone.
- High-intensity statin: Atorvastatin 80 mg daily. Cuts cholesterol hard and stabilizes artery plaques.
- Blood pressure control: Target under 140/90. If you’re diabetic, even lower.
Some hospitals now use telemedicine TIA clinics. You get a video consult with a stroke specialist within hours. No waiting. No driving. Just fast, expert care. That’s how you beat the clock.
Why ‘mini-stroke’ is a lie
Calling a TIA a ‘mini-stroke’ is like calling a fire alarm a ‘mini-fire.’ It’s misleading. It makes people ignore the danger.
The American Heart Association stopped using the term ‘mini-stroke’ in 2009. They now define a TIA by brain tissue damage-not how long symptoms last. If there’s no infarction on MRI, it’s a TIA. If there is? It’s a stroke. Even if the symptoms vanished in 10 minutes.
Doctors at Mayo Clinic and St. Vincent’s Hospital say the same thing: If your brain didn’t get blood for even a few minutes, it’s an emergency. The fact that you feel fine now doesn’t mean your body is fine. Your arteries are still damaged. Your blood is still clotting. Your risk hasn’t disappeared. It’s just waiting.
What you can do right now
You don’t need to be a doctor to save a life. Here’s what you do:
- If you or someone has sudden face drooping, arm weakness, speech trouble-call 911. Even if it’s gone.
- Don’t drive yourself. Don’t wait. Emergency responders can start treatment in the ambulance.
- Bring a list of medications, allergies, and medical history. It saves time.
- After the hospital visit, follow up with a neurologist. Don’t skip it.
- Control your blood pressure, quit smoking, manage diabetes, and get moving. Lifestyle changes cut your stroke risk by half.
And if you’ve ever brushed off dizziness or slurred speech as ‘just tired’ or ‘stress’-stop. That’s how strokes happen. TIA is your body’s last chance to tell you before it’s too late.
What happens if you ignore it?
Ignoring a TIA isn’t just risky. It’s costly-financially and physically.
The average cost of treating a TIA? Around $2,850. The average cost of treating a stroke? Over $21,000. And that’s just the hospital bill. Add rehab, home care, lost income, long-term support. The total lifetime cost of a stroke can hit $150,000.
But the real cost? The life you lose. Or the life you can’t live the same way again. One in five TIA survivors will have a stroke. One in five. And of those, 25% will die within a year. Another 30% will need help walking, talking, or feeding themselves.
Hospitals that follow strict TIA protocols-like the SOS-TIA program at Massachusetts General-cut 90-day stroke risk from 10% to just 1.2%. That’s not magic. That’s speed. That’s action.
What’s changing in stroke care?
The science is moving fast. In 2022, researchers at UC San Francisco found that a simple blood test for GFAP-a protein released when brain cells are injured-could tell if someone had a stroke or TIA in under 15 minutes. Right now, it’s 48% accurate. By 2026, it’s expected to hit 85%. That means in the future, ER doctors might know within minutes if you’re having a stroke-even before imaging.
AI tools are also getting better. One model in California can predict stroke risk after a TIA with 92% accuracy by analyzing MRI scans and patient history. That’s better than most doctors can do alone.
And Medicare is now penalizing hospitals if more than 20% of TIA patients have a stroke within 30 days. That’s forcing every emergency room to take TIA seriously. No more waiting. No more dismissals.
Final thought: Don’t wait for it to come back
Most people think stroke only happens to older people. It doesn’t. It happens to people who ignore warning signs. It happens to people who think, ‘I’ll check it out tomorrow.’
A TIA is not a warning. It’s the beginning of a stroke that didn’t finish. And if you let it go, the next one will.
Know the signs. Act fast. Call 911. Even if it’s gone. Even if you feel fine. Your brain doesn’t lie. And neither should you.


Gus Fosarolli
November 28, 2025 AT 20:38My uncle ignored his TIA. Thought he was 'just tired.' Two days later, he couldn’t speak. Now he needs help eating. Don’t be him.
Evelyn Shaller-Auslander
November 30, 2025 AT 03:52Jill Ann Hays
December 1, 2025 AT 04:53Mike Rothschild
December 1, 2025 AT 17:24Ron Prince
December 3, 2025 AT 09:21Sarah McCabe
December 4, 2025 AT 20:30King Splinter
December 6, 2025 AT 04:15Kristy Sanchez
December 8, 2025 AT 01:36Michael Friend
December 9, 2025 AT 18:40Jerrod Davis
December 11, 2025 AT 09:42Dominic Fuchs
December 12, 2025 AT 00:30Asbury (Ash) Taylor
December 13, 2025 AT 11:40Kenneth Lewis
December 14, 2025 AT 06:30Jim Daly
December 15, 2025 AT 01:25Tionne Myles-Smith
December 15, 2025 AT 13:56