Introduction to Allergic Conjunctivitis and Climate Change
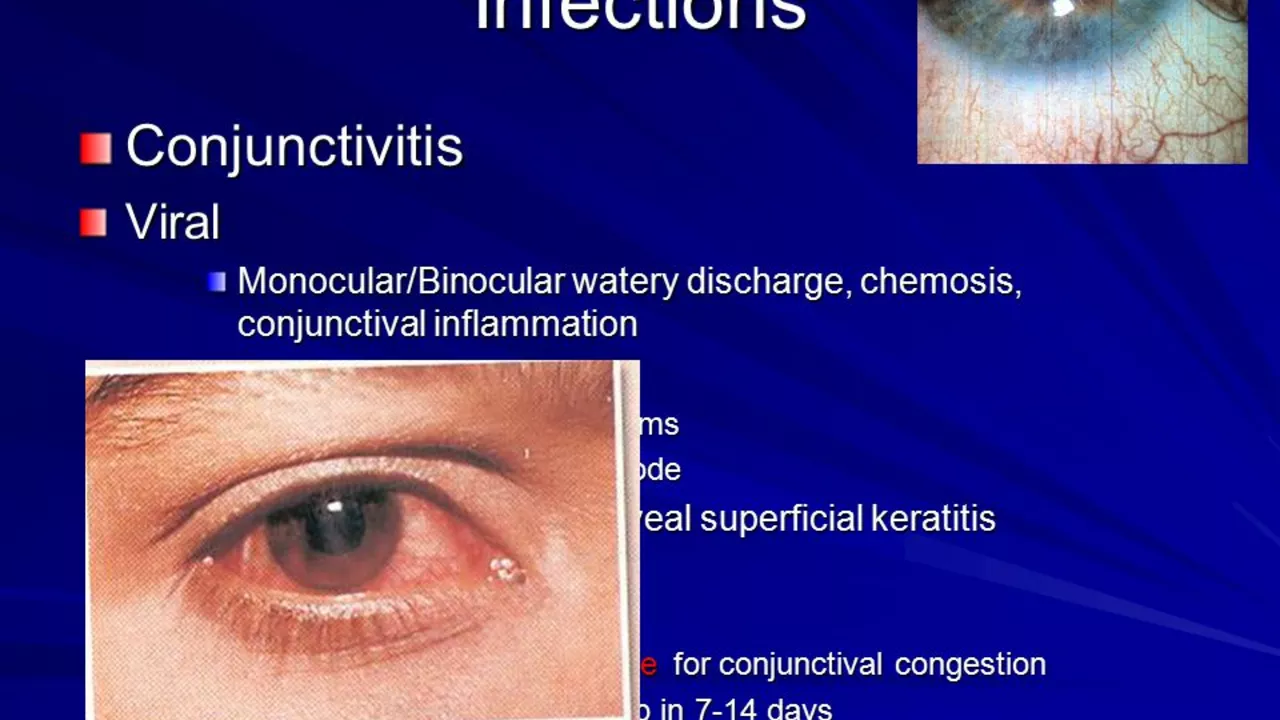
As a blogger who is passionate about environmental and health issues, I have noticed a growing concern regarding the impact of climate change on the prevalence of allergic conjunctivitis. Allergic conjunctivitis, also known as pink eye, is a common eye condition that causes inflammation, itching, and redness. It is primarily caused by allergens in the environment, such as pollen, dust mites, and pet dander. In this article, we will explore the various ways climate change is affecting the occurrence of allergic conjunctivitis and what we can do to mitigate its effects.
Increasing Pollen Levels and Longer Pollen Seasons
One of the main factors contributing to the rise in allergic conjunctivitis cases is the increase in pollen levels due to climate change. As temperatures rise, plants are able to produce pollen for longer periods, leading to longer pollen seasons. In addition, higher levels of carbon dioxide in the atmosphere stimulate plants to produce more pollen. This means that there is not only more pollen in the air, but it is also present for a longer period of time, increasing the risk of allergic conjunctivitis for those who are susceptible to pollen allergies.
Greater Geographic Spread of Allergenic Plants
Climate change is also causing allergenic plants to spread to new areas where they were not previously found. As temperatures rise, these plants are able to thrive in regions that were once too cold for them. This means that people who were not previously exposed to these allergens are now at risk of developing allergic conjunctivitis. The greater geographic spread of allergenic plants also increases the overall number of people who are exposed to these allergens, further raising the prevalence of allergic conjunctivitis.
Increased Exposure to Indoor Allergens
As climate change leads to more extreme weather events, such as heatwaves and storms, people are spending more time indoors. This increased time spent indoors can lead to greater exposure to indoor allergens, such as dust mites and pet dander, which are common triggers for allergic conjunctivitis. Furthermore, higher temperatures and humidity levels can increase the growth and reproduction of these allergens, making them more prevalent in indoor environments.
Greater Risk of Mold Allergies
Climate change is also contributing to a greater risk of mold allergies, which can trigger allergic conjunctivitis. Warmer temperatures and increased humidity create the perfect environment for mold to grow, both indoors and outdoors. As mold spores are released into the air, they can come into contact with the eyes, causing an allergic reaction and the onset of conjunctivitis symptoms.
Higher Air Pollution Levels
Higher air pollution levels, which are partially caused by climate change, can also contribute to the prevalence of allergic conjunctivitis. Air pollutants, such as particulate matter and ozone, can irritate the eyes and exacerbate allergy symptoms. In addition, these pollutants can interact with allergens, making them more potent and increasing the risk of allergic reactions.
Increased Vulnerability in Developing Countries
Developing countries are particularly vulnerable to the impacts of climate change, including the increased prevalence of allergic conjunctivitis. These countries often lack the resources and infrastructure to adequately address the health issues caused by climate change. This, combined with factors such as poor air quality, overcrowding, and limited access to healthcare, can lead to a higher number of people suffering from allergic conjunctivitis in these regions.
Adapting to the Changing Climate
As we continue to experience the effects of climate change, it is crucial that we adapt our lifestyles and healthcare practices to mitigate the impacts on allergic conjunctivitis prevalence. This can include implementing strategies to reduce indoor allergens, such as using air purifiers and regularly cleaning surfaces where allergens may accumulate. It is also important to stay informed about local pollen levels and take appropriate precautions, such as wearing protective eyewear and avoiding outdoor activities during peak pollen times.
Conclusion: The Need for Action on Climate Change
In conclusion, the impact of climate change on the prevalence of allergic conjunctivitis is a significant and growing concern. As temperatures rise, pollen seasons become longer, allergenic plants spread to new regions, and air pollution increases, we are likely to see a greater number of people affected by this condition. It is crucial that we take action to address the root causes of climate change and work to mitigate its effects on our health and well-being. By doing so, we can help to reduce the prevalence of allergic conjunctivitis and improve the overall quality of life for those who suffer from this condition.

Leslie Woods
June 18, 2023 AT 23:00I’ve been noticing the pollen count creeping up every spring and it’s not just me – my eyes get that itchy sting way sooner now. The longer seasons mean we’re exposed to allergen particles for weeks we never used to have. It also lines up with those hotter summers that keep plants buzzing. If we keep ignoring the link between climate shifts and eye irritation we’ll just keep reaching for the drops.
Manish Singh
June 19, 2023 AT 01:13I totally feel you leslie its like the air itself is a sneeze factory now. Also many folks in developing areas dont have easy access to proper eye care which makes the problem even worse. We need community level education about indoor cleaning and maybe some low‑cost air filters. Keep spreading the word!
Dipak Pawar
June 19, 2023 AT 06:46The phenomenology of allergic conjunctivitis in the Anthropocene is underpinned by a complex interplay of aero‑allergen dynamics and thermally driven phenological shifts.
Elevated atmospheric CO₂ concentrations act as a potent fertilization agent, augmenting the biosynthetic pathways of pollen‑producing anemophilous taxa.
Consequently, pollen grains exhibit increased allergenicity due to heightened protein expression, notably profilin and Phl p 5 homologs.
Extended thermal windows further elongate the anthesis period, resulting in a protracted dispersal timeline that surpasses historical baselines.
Geospatial analyses reveal a poleward and altitudinal migration of ragweed, birch, and other high‑impact species, facilitated by microclimatic niches emerging in previously inhospitable zones.
These biogeographic incursions expose naïve immunological cohorts to novel epitope repertoires, precipitating de‑novotranscriptional sensitization events.
Urban heat islands exacerbate the situation by creating localized hyperthermal pockets where pollen viability and release rates are maximized.
Simultaneously, particulate matter (PM₂.₅) and ozone act synergistically with pollen, forming adducts that enhance mucosal permeability and inflammatory cascade activation.
Indoor environments are not exempt; higher humidity levels foster proliferation of Dermatophagoides spp. and mold spores, both of which serve as co‑factors in conjunctival hyperreactivity.
In low‑resource settings, limited access to allergen‑specific immunotherapy and suboptimal housing conditions amplify disease burden.
From a public health perspective, integrated surveillance systems that couple aerobiological monitoring with climate modeling are imperative.
Policy interventions must prioritize emission reductions, urban greening with low‑allergen flora, and the dissemination of affordable protective eyewear.
Clinicians should counsel patients on temporal avoidance strategies, such as scheduling outdoor activities during mid‑day lulls in pollen release.
Research agendas ought to explore genetically attenuated cultivars and bio‑engineered phytoremediators capable of sequestering airborne allergens.
Ultimately, mitigating the climatological drivers of allergic conjunctivitis requires a transdisciplinary coalition spanning climatology, botany, immunology, and socio‑economic planning.
Jonathan Alvarenga
June 19, 2023 AT 12:20Dipak’s deep dive into the mechanistic pathways is academically impressive but it reads like a textbook marathon that leaves most readers gasping for a simple takeaway. The sheer volume of jargon makes it hard to extract practical advice for the everyday sufferer. While the precision is commendable, a concise executive summary would serve the community far better. In short, cut the fluff and hand us the actionable steps.
Jim McDermott
June 19, 2023 AT 20:40I’m with you Jim – the rising pollen really does feel like nature’s own eye irritant. I’ve started checking local pollen forecasts on my phone and it helps me plan my outdoor runs. Also, using a humidifier at night seems to keep the indoor dust mite count down. Just a few tweaks can make a big difference.
Naomi Ho
June 20, 2023 AT 03:36Here are a few practical steps you can try right away – keep windows closed during peak pollen hours run a HEPA filter in the bedroom dust surfaces with a damp cloth use preservative‑free eye drops regular cleaning of bedding and curtains can lower indoor allergen load These simple habits often reduce symptoms noticeably
Christine Watson
June 20, 2023 AT 10:33It’s heartening to see so many of us banding together to tackle this hidden side effect of climate change. Even small actions like wearing sunglasses on windy days can protect our eyes and raise awareness. Let’s keep the conversation alive and share what works for us.
Macy Weaver
June 20, 2023 AT 17:30I love the optimism you bring Christine and I’d add that community workshops on allergen‑free gardening can empower neighbors to create safer outdoor spaces. Sharing plant lists and low‑cost filter tips in local groups spreads the knowledge fast.
James McCracken
June 21, 2023 AT 00:26Surely the elite think pollen is just a minor inconvenience.
Evelyn XCII
June 21, 2023 AT 07:23Oh absolutely Evelyn your sarcasm really brightens the discussion like a fresh breeze of pollen.
Suzanne Podany
June 21, 2023 AT 14:20Everyone dealing with allergic conjunctivitis deserves access to clear information and effective tools. Let’s mentor each other on the best cleaning routines, share reliable resources, and advocate for cleaner air policies together.
Nina Vera
June 21, 2023 AT 22:40WOW NINA this thread is like a storm of ideas and I’m riding the wave! The passion here is contagious and I’m pumped to jump in with my own tips and hype up the fight against climate‑driven eye woes!