Understanding Childhood Trauma
In order to discuss the impact of childhood trauma on depression in adulthood, it's crucial to first understand what constitutes childhood trauma. Childhood trauma is a distressing experience or set of experiences that occur during one's formative years. It could be physical, emotional, or sexual abuse, neglect, or witnessing violence or severe discord in the family. It's important to note that trauma can be subjective; what may be traumatic for one child may not be for another. However, the effect of these distressing experiences can be profound and long-lasting, shaping the way an individual interacts with the world as an adult.
The Connection between Childhood Trauma and Adult Depression
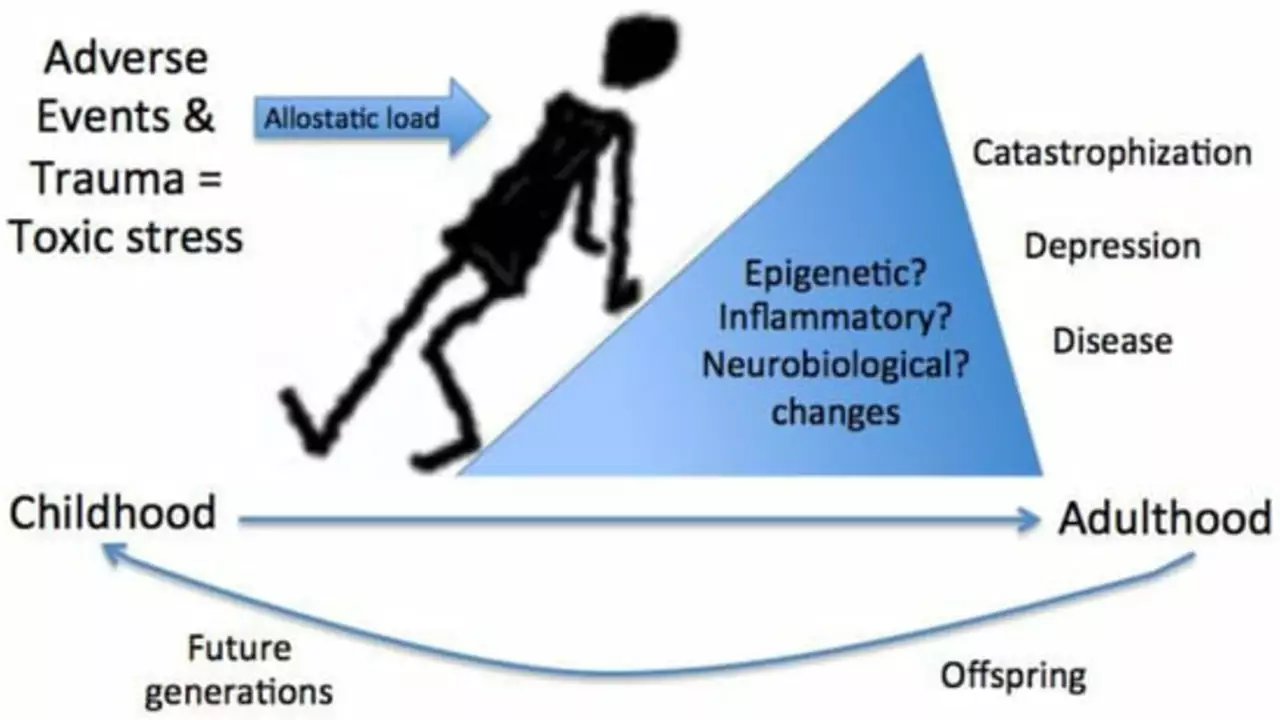
Research has consistently found a significant correlation between childhood trauma and the development of depression in adulthood. This doesn't mean that every individual who experiences childhood trauma will inevitably develop depression, but they are at a higher risk. The trauma disrupts the normal development of certain brain structures and functions, making the individual more susceptible to mental health disorders such as depression.
How Childhood Trauma Influences Brain Development
Childhood is a critical period for brain development, and traumatic experiences during this time can cause significant alterations. This can result in chronic hyperarousal, where the brain is constantly on high alert for danger, leading to anxiety and depression. Moreover, trauma can disrupt the development of the prefrontal cortex, which is responsible for regulating emotions and decision-making, making it harder to cope with stress and increasing the risk of depression.
Childhood Trauma and the Body's Stress Response
Childhood trauma can also affect the body's stress response system, leading to an overactive stress response. This can result in chronic inflammation, which has been linked to depression. An overactive stress response can also lead to sleep problems and other physical health issues, which can further contribute to depression.
Attachment and Childhood Trauma
Childhood trauma can disrupt the formation of secure attachments, which are crucial for emotional development and mental health. Children who experience trauma may have difficulty forming healthy relationships as adults, which can lead to feelings of isolation and contribute to depression.
Self-Esteem and Childhood Trauma
Children who experience trauma may develop a negative self-concept, believing that they are unworthy or unlovable. This can persist into adulthood, leading to low self-esteem and depression. Having a negative self-image can also make it harder to form healthy relationships, further contributing to feelings of isolation and depression.
The Role of Resilience in Overcoming Childhood Trauma
Not all children who experience trauma go on to develop depression. Resilience, or the ability to bounce back from adversity, can be a protective factor. Factors that contribute to resilience include having at least one supportive adult in the child's life, developing coping skills, and having a sense of purpose or future orientation.
Treatment Options for Adults with Childhood Trauma
Fortunately, there are effective treatments available for adults who have experienced childhood trauma and are struggling with depression. These include various forms of therapy, such as cognitive-behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), and trauma-focused cognitive-behavioral therapy (TF-CBT). Antidepressants can also be effective in managing symptoms of depression.
Preventing Childhood Trauma and its Long-Term Effects
Prevention is always better than cure. Efforts should be made to prevent childhood trauma, such as implementing parenting programs, providing support for families in crisis, and promoting awareness of child abuse and neglect. However, when prevention fails, early intervention is crucial to mitigate the long-term effects of trauma.
Conclusion: The Lasting Impact of Childhood Trauma
In conclusion, childhood trauma can have a profound impact on an individual's mental health in adulthood, increasing the risk of depression. Understanding this connection can help in the development of prevention strategies, early intervention programs, and effective treatments. Despite the challenges, it's important to remember that recovery is possible, and with the right support and treatment, individuals who have experienced childhood trauma can lead fulfilling, healthy lives.

Andy McCullough
July 26, 2023 AT 21:21From a neurobiological standpoint, early adverse experiences precipitate dysregulation of the hypothalamic‑pituitary‑adrenal (HPA) axis, leading to heightened cortisol output. This hypercortisolemic state can induce epigenetic modifications that alter transcriptional profiles of genes implicated in mood regulation, such as BDNF and NR3C1. Moreover, longitudinal neuroimaging studies demonstrate reduced gray matter volume in the prefrontal cortex and aberrant amygdala connectivity among trauma‑exposed cohorts. Such structural and functional maladaptations compromise top‑down emotional regulation, thereby increasing susceptibility to major depressive disorder. In addition, chronic inflammation-mediated by elevated cytokines like IL‑6 and TNF‑α-serves as a peripheral conduit linking early stress to affective pathology. The cumulative effect of these mechanisms underscores why childhood trauma is a robust predictive factor for adult depression. Clinically, this informs the utility of trauma‑focused interventions that target both neuroendocrine and psychosocial domains. Ultimately, integrating biomarkers with psychotherapeutic modalities offers a translational pathway to mitigate long‑term sequelae.
Zackery Brinkley
July 27, 2023 AT 08:28That overview really underscores why compassionate support is essential.
Luke Dillon
July 27, 2023 AT 19:35Hey, I appreciate how you laid out the connection between early stress and later mood swings in plain language. It can be overwhelming to hear that trauma reshapes the brain, but knowing the science gives us a foothold for recovery. The piece also highlights that not everyone who’s been hurt ends up depressed, which is hopeful. Keep sharing these insights-they help demystify a tough subject.
Elle Batchelor Peapell
July 28, 2023 AT 06:41Man, reading about childhood trauma feels like staring into a cracked mirror that still reflects our present. You know, it’s wild how those early cracks can echo louder than any adult heartbreak. When a kid grows up with constant fear, their brain learns to treat every whisper as a scream. That hyper‑alert mode becomes a default setting, and suddenly normal stress feels like a hurricane. But what blows my mind is how those same neural pathways that guard us from danger also lock us out of joy. It’s like your mind built a fortress to keep the bad guys out, but now the doors stay shut on anyone who wants to come in. We end up scrolling through life with a soundtrack of “what if” and “I’m not good enough” on repeat. At the same time, resilience is this stubborn weed that can sprout even in concrete cracks. Having one caring adult, learning a coping skill, or finding a purpose can act like sunlight breaking through the gloom. Therapies like CBT or EMDR are basically tools to rewire those old alarm systems, teaching the brain that it’s safe to relax. And let’s not forget that the body’s stress response isn’t just in the head; chronic inflammation can literally make you feel physically miserable. That’s why sleep problems and aches often tag along with the emotional weight. The good news is that science is finally catching up, showing us how to target both mind and body in treatment. So, while the scars of childhood can run deep, they’re not immutable-our brains stay plastic longer than most of us think. Every therapy session, every supportive conversation, is like chipping away at the marble to reveal a smoother shape underneath. Bottom line: trauma shapes us, but we also have the tools to reshape ourselves, and that’s something worth fighting for.
Jeremy Wessel
July 28, 2023 AT 12:15Trauma leaves marks but change is possible. Simple steps matter. Support can shift outlook. Therapy rewires patterns. Hope grows with effort.
Laura Barney
July 28, 2023 AT 17:48Think of trauma as a storm that drenches the soul, yet the rainbow that follows is painted by the very same clouds that once wept. Your words shine a vivid light on how resilience can bloom even in the darkest soil, turning bruised hearts into wild gardens of strength. I love how you blend raw honesty with a splash of optimism, making the heavy subject feel like a canvas ready for bold strokes. It’s a reminder that we’re not just victims of our past but architects of our future, building bridges from broken pieces. Keep spilling this kaleidoscopic truth-it’s exactly the color we need.
Jessica H.
July 29, 2023 AT 02:08The preceding passage, while evocatively crafted, risks over‑generalizing the therapeutic trajectory by implying uniform outcomes across heterogeneous populations. Empirical literature underscores considerable variability in treatment response contingent upon factors such as comorbid conditions, socioeconomic status, and genetic predispositions. Moreover, the metaphorical language, though engaging, may obscure the nuanced mechanisms by which cognitive‑behavioral interventions exert neurobiological effects. A more balanced articulation would integrate statistical variance and acknowledge the limits of resilience as a protective factor. Nonetheless, the overall synthesis aligns with current consensus regarding the importance of early, tailored interventions.
Tom Saa
July 29, 2023 AT 07:41It’s intriguing how early stress rewires the circuitry that later governs affect, almost as if the brain writes its own cautionary tale. Yet, within that deterministic framing, there lies a paradox: the same plasticity that cements vulnerability also offers a gateway for re‑learning, suggesting that the narrative isn’t sealed. Perhaps the key resides not in erasing the past imprint but in overlaying it with new, adaptive scripts.
John Magnus
July 29, 2023 AT 18:48Let’s cut the fluff: the data is unequivocal-childhood adversity amplifies the odds of major depressive episodes by a factor that cannot be dismissed as mere correlation. Meta‑analyses reveal effect sizes approaching 0.5 to 0.7, indicating a robust relationship that survives even after controlling for socioeconomic confounds. Ignoring this link in clinical practice is tantamount to malpractice, because it blinds providers to a principal etiological driver. Therefore, comprehensive assessment protocols must mandate trauma screening as a non‑negotiable baseline. Anything less is a dereliction of duty.
Marc Clarke
July 30, 2023 AT 05:55Wow, that was a deep dive and honestly, it gives me a lot of hope. Knowing that the brain can still grow and adapt, even after tough years, feels like a reminder that we’re not stuck. Plus, the stories about supportive adults and coping skills make the whole thing feel doable. It’s cool to see science and real‑life tips blend together. Keep the good vibes coming, and thanks for breaking it down.
angelica maria villadiego españa
July 30, 2023 AT 17:01Reading this really shows how important it is to reach out and listen to those who have been hurt. Simple acts of kindness can make a big difference in someone’s recovery journey. It’s comforting to know that help is out there and that healing is possible.