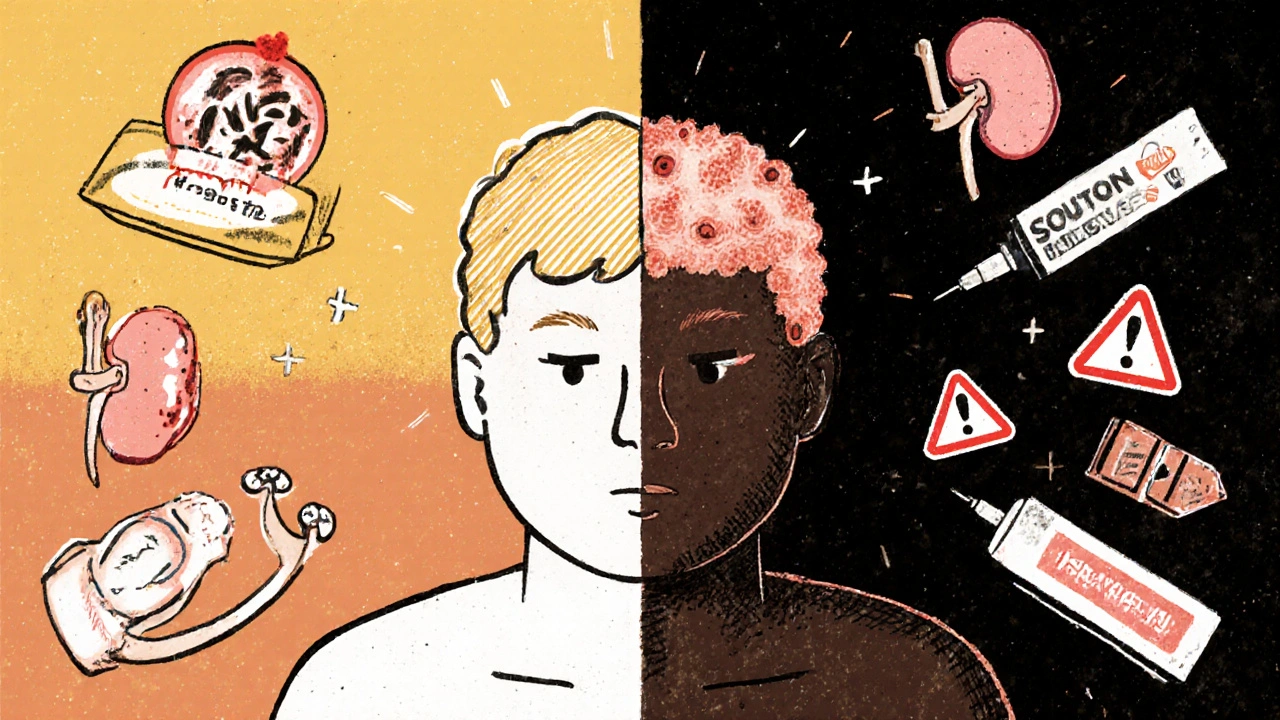
Systemic lupus erythematosus (SLE) isn’t just one disease-it’s a shifting puzzle that affects different people in wildly different ways. One person might struggle with a butterfly-shaped rash across their cheeks, while another battles kidney failure or crushing fatigue that no amount of sleep fixes. It’s autoimmune, meaning the body turns on itself, attacking healthy tissue like skin, joints, kidneys, and even the brain. And while it can show up at any age, it hits hardest in women between 15 and 45, especially those of Black, Asian, or Hispanic descent. In Australia, where sunlight is strong and winters are mild, lupus flares tied to UV exposure are common. The good news? We know more now than ever about how to manage it-and many people with SLE live full, active lives.
What Does Lupus Actually Do to Your Body?
Lupus doesn’t stick to one organ. It’s a systemic disease, meaning it can wander through your body like an uninvited guest. The most common signs show up in the skin, joints, and blood. About 95% of people with SLE will have joint pain or swelling at some point-often mistaken for arthritis. Fatigue hits 9 out of 10 patients, not the kind you shake off after a good night’s sleep, but a deep, bone-tired exhaustion that doesn’t improve with rest.
The classic malar rash-the butterfly-shaped redness across the nose and cheeks-is what most people picture. But it’s not the only skin sign. Discoid lupus leaves thick, scaly patches that scar and can cause permanent hair loss if they appear on the scalp. Then there’s subacute cutaneous lupus, a photosensitive rash that looks like red, scaly rings or patches, often triggered by sun exposure. People with this form usually test positive for Anti-Ro (SSA) antibodies. Even less common forms like chilblains lupus (painful purple bumps on fingers and toes in cold weather) or lupus panniculitis (deep, sunken lumps under the skin) show how wide the spectrum is.
Inside the body, lupus can attack the kidneys in about half of patients, leading to lupus nephritis. This is serious-it can lead to kidney failure if not caught early. That’s why regular urine tests and blood creatinine checks every three months are non-negotiable. Blood problems are also common: low red blood cells (anemia), low white blood cells (leukopenia), and low platelets (thrombocytopenia) all happen because the immune system destroys them. Heart and lung involvement isn’t rare either. Pleuritis (inflammation around the lungs) and pericarditis (around the heart) cause sharp chest pain that gets worse when breathing deeply. About 1 in 4 people with lupus will develop cardiovascular disease, often earlier than expected.
What Triggers a Lupus Flare?
A flare is when symptoms suddenly get worse. Sometimes it’s obvious-like a rash spreading after a day at the beach. Other times, it creeps in: more joint pain, a spike in fatigue, or a fever with no infection. Flares can be mild or life-threatening. The triggers? Some are clear, others still mysterious.
Sunlight is the biggest known trigger for skin and systemic flares. UV rays confuse the immune system, making it attack skin cells and release inflammatory signals. That’s why daily use of SPF 50+ sunscreen and wide-brimmed hats isn’t optional-it’s medical advice. Certain medications can also trigger lupus-like symptoms, especially hydralazine (for high blood pressure), procainamide (for heart rhythm), and isoniazid (for tuberculosis). These are rare, and the symptoms usually go away when you stop the drug. Hydrochlorothiazide, a common diuretic, is linked to subacute cutaneous lupus.
Pregnancy is another major trigger. About 30% of women with SLE experience a flare during pregnancy, and risks like preeclampsia, preterm birth, and miscarriage go up. That’s why planning ahead is critical. Ideally, you should be in remission for at least six months before trying to conceive. Stress doesn’t show up on blood tests, but patients and doctors alike see the connection. High stress levels often precede flares, even if we can’t measure it exactly.
How Is Lupus Diagnosed?
There’s no single test for lupus. Diagnosis is like putting together a jigsaw puzzle with pieces from symptoms, blood tests, and medical history. The 2019 classification criteria from the American College of Rheumatology and EULAR require a positive antinuclear antibody (ANA) test as the entry point. Nearly everyone with SLE has a positive ANA-it’s sensitive, but not specific. Many healthy people have it too.
More telling are the specific antibodies. Anti-dsDNA is found in 60-70% of SLE patients and often rises during flares. Anti-Smith is rarer (20-30%) but almost exclusive to lupus, making it a strong diagnostic clue. Antiphospholipid antibodies are important too-they raise the risk of blood clots and miscarriages. If you have these, your doctor might recommend low-dose aspirin or blood thinners.
Clinical signs matter just as much. A positive ANA plus two or more of these: malar rash, discoid rash, oral ulcers, arthritis, kidney involvement, neurological symptoms, or blood count abnormalities, can confirm the diagnosis. The system gives points to each feature, and a total score of 10 or more means SLE. It’s not perfect, but it’s the best tool we have.
How Is Lupus Managed?
There’s no cure-but there’s control. The goal isn’t just to treat symptoms; it’s to reach low disease activity or remission and prevent long-term organ damage. Treatment is personalized. What works for one person might not help another.
Hydroxychloroquine (Plaquenil) is the foundation for nearly everyone with SLE. It’s not a steroid. It doesn’t cause weight gain or mood swings. Instead, it calms the immune system, reduces flares by about 50%, lowers the risk of blood clots, and even improves survival. Doctors recommend a daily dose of 5 mg per kilogram of body weight-no more, no less. Too much can harm the eyes, so annual eye exams are required. If you’re not on hydroxychloroquine, ask why.
For skin rashes, topical steroids or antimalarials applied directly help. For joint pain and mild inflammation, nonsteroidal anti-inflammatory drugs (NSAIDs) like naproxen are often enough. But if the disease hits the kidneys, lungs, brain, or blood, you need stronger drugs. Corticosteroids like prednisone are fast-acting but come with serious side effects over time-bone loss, diabetes, weight gain. For severe flares, doctors may give high-dose intravenous methylprednisolone for three days to quickly shut down inflammation.
For organ-threatening disease, immunosuppressants are essential. Mycophenolate mofetil (Cellcept) is now the first choice for lupus nephritis, with 60-70% of patients showing major kidney improvement. Azathioprine (Imuran) and cyclophosphamide are older options, still used in specific cases. For patients who don’t respond, rituximab (Rituxan) targets B-cells, the immune cells that make harmful antibodies.
Newer drugs are changing the game. Anifrolumab, approved in 2021, blocks type I interferon-a key driver of inflammation in lupus. In trials, it cut disease activity scores by 40-50%. Other drugs in development target JAK enzymes, BTK proteins, and other specific immune pathways. Personalized treatment based on biomarkers is the next frontier.
What Can You Do Every Day to Stay Well?
Medication is only part of the story. Daily habits make a huge difference.
- Sun protection: Wear UPF 50+ clothing, broad-spectrum SPF 50+ sunscreen every day-even on cloudy days. Avoid direct sun between 10 a.m. and 4 p.m.
- Exercise: Gentle aerobic activity like walking, swimming, or cycling improves fatigue in 65% of patients. Start slow. Even 20 minutes a day helps.
- Rest: Prioritize sleep. Fatigue isn’t laziness-it’s your body signaling it needs recovery.
- Quit smoking: Smoking increases heart disease risk, which is already high in lupus. It also makes some medications less effective.
- Manage stress: Yoga, meditation, or even regular walks in nature can lower flare risk. Don’t ignore emotional health.
- Monitor your body: Keep a symptom journal. Note rashes, pain levels, energy, and mood. Bring it to appointments.
Regular blood and urine tests every three months catch kidney problems early. Blood pressure and cholesterol checks are just as important-heart disease is the leading cause of death in SLE.

What’s the Long-Term Outlook?
Twenty years ago, lupus was often fatal. Today, 80-90% of people with SLE live a normal lifespan. That’s thanks to better drugs, earlier diagnosis, and smarter management. But survival isn’t the same as quality of life.
People with lupus nephritis have an 88% 10-year survival rate-slightly lower than those without kidney involvement. The biggest threats? Heart disease (30-40% of deaths), infections (20-25%), and active disease (10-15%). Black and Hispanic patients still face 2-3 times higher death rates than White patients, due to delays in diagnosis, access to care, and biological differences.
Childhood-onset lupus (affecting about 20% of patients) tends to be more aggressive. Eight in ten kids have major organ damage at diagnosis. That’s why early, aggressive treatment is critical.
The future is promising. Research is moving beyond broad immunosuppression to targeted therapies. We’re learning how to predict flares before they happen. We’re finding which patients will respond to which drugs. The goal isn’t just to survive lupus-it’s to live well with it.
Can you outgrow lupus?
No, lupus is a lifelong condition. Even if symptoms disappear for months or years, the immune system still carries the tendency to attack the body. That’s why staying on maintenance medication like hydroxychloroquine is so important-even when you feel fine. Stopping it increases flare risk by up to 50%.
Is lupus hereditary?
Lupus isn’t directly inherited like a genetic disorder, but having a close relative with lupus or another autoimmune disease (like rheumatoid arthritis or thyroiditis) increases your risk. Certain genes related to immune function-like those involved in clearing dead cells or regulating interferon-play a role. But genes alone don’t cause it. Environmental triggers like sunlight, infections, or stress are needed to turn on the disease.
Can you have lupus without a positive ANA?
It’s extremely rare. Nearly all people with SLE have a positive ANA test. If ANA is negative and symptoms strongly suggest lupus, doctors will look for other causes-like other autoimmune diseases or infections. In very rare cases, a person might test negative early on and become positive later. If suspicion is high, the test may be repeated.
Does diet affect lupus?
There’s no proven "lupus diet," but what you eat can help manage symptoms and reduce inflammation. Omega-3 fatty acids (from fish, flaxseeds, walnuts) may lower inflammation. Avoiding processed foods, excess sugar, and saturated fats helps control weight and heart risk. Some people find that alfalfa sprouts or garlic trigger flares-these contain compounds that can overstimulate the immune system. Always talk to your doctor before starting supplements.
Can women with lupus have healthy pregnancies?
Yes, but planning is everything. The best outcomes happen when lupus has been stable for at least six months before conception. Medications like hydroxychloroquine and low-dose prednisone are safe during pregnancy. Avoid drugs like cyclophosphamide or mycophenolate-they’re harmful to the fetus. Regular monitoring by a rheumatologist and high-risk OB is essential. Most women with well-controlled lupus deliver healthy babies.
What happens if I stop taking my lupus meds?
Stopping medication without medical advice is risky. Hydroxychloroquine reduces flares by half-quitting doubles your chance of a flare. Stopping steroids too quickly can cause a rebound flare or adrenal crisis. Immunosuppressants need to be tapered slowly. Even if you feel great, your disease might still be quietly active. Always work with your doctor to adjust or stop any treatment.
What Comes Next?
If you’ve been diagnosed with SLE, your next steps are simple but vital. First, get on hydroxychloroquine if you’re not already. Second, schedule your annual eye exam. Third, start tracking your symptoms in a journal. Fourth, talk to your doctor about your sun protection plan. Fifth, connect with a rheumatologist who specializes in lupus-not just any doctor.
Don’t wait for a flare to act. Prevention is the best treatment. And if you’re a caregiver, family member, or friend-understand that fatigue isn’t laziness, and invisible symptoms are still real. Support matters as much as medicine.
The science is advancing fast. New drugs are coming. Better tests are on the horizon. For now, the message is clear: with the right care, you can live fully with lupus. You’re not defined by your diagnosis-you’re defined by how you manage it.


Jim Oliver
November 10, 2025 AT 17:19Let me just say-hydroxychloroquine isn't a 'supplement,' it's a backbone treatment. If your doctor isn't prescribing it, they're either lazy or misinformed. And yes, you need the annual eye exam. No, your 'I feel fine' doesn't override retinal toxicity risk. Stop making excuses.
William Priest
November 11, 2025 AT 19:07so like… lupus is just your immune system having a bad day? lol. i mean, i get it’s serious but like… why do people act like it’s magic? also hydroxychloroquine sounds like a drug from a 90s sci fi movie. why not just take turmeric? 🤔
Ryan Masuga
November 13, 2025 AT 02:41Hey, just wanted to say this post was super helpful. I’ve got a friend with lupus and I never realized how much goes into managing it. The part about daily sun protection really hit home-I always thought sunscreen was just for beach days. Now I’m gonna start reminding her to reapply. Small things matter. Keep sharing this stuff.
Jennifer Bedrosian
November 13, 2025 AT 08:37OMG I just read this and I’m crying. I had a flare last month and my doctor just told me to ‘rest more’ and gave me ibuprofen. Like… what? I’ve been researching for weeks and this is the first time someone actually explained what’s happening inside my body. Thank you. I’m not crazy. I’m not lazy. I’m just fighting a silent war.
Lashonda Rene
November 13, 2025 AT 23:12you know i think a lot of people dont understand how hard it is to live with something invisible. like you look fine on the outside but inside your body is basically at war. and the fatigue? its not just being tired. its like your bones are filled with wet cement and you have to drag yourself through the day. and then people say ‘why dont you just exercise more’ like its that easy. i wish everyone could feel what we feel for just one day.
Andy Slack
November 15, 2025 AT 14:14Hydroxychloroquine is non-negotiable. If you’re not on it, you’re playing Russian roulette with your organs. And yes, the eye exams are boring but they save your vision. Do the work. Your future self will thank you.
Rashmi Mohapatra
November 16, 2025 AT 13:39so many people in India dont even know what lupus is. they think its just a rash or allergy. my cousin had it for 3 years and no one believed her. doctors said she was stressed. now she has kidney damage. why is awareness so low here? this post should be translated to Hindi and Tamil. people need to know.
Abigail Chrisma
November 17, 2025 AT 11:03Thank you for writing this with so much care. I’m a Black woman with lupus and I’ve been told my pain was ‘emotional’ or ‘exaggerated.’ This post validates what we live every day. To anyone reading this: your experience is real. Your fatigue is real. Your fight is real. And you’re not alone.
Ankit Yadav
November 18, 2025 AT 19:44One thing missing here is the cost of care. Hydroxychloroquine is cheap but the blood tests, rheumatologist visits, and specialty meds? In the US, insurance won’t cover it all. Many people skip tests because they can’t afford them. That’s why mortality rates are higher for low-income patients. Treatment isn’t just about pills-it’s about access.
Meghan Rose
November 20, 2025 AT 16:45I’m sorry but I have to say this-I’ve read every single word of this and I still think the whole lupus narrative is overblown. I mean, look at the stats-80-90% survival rate? That’s basically a chronic cold. Why do people act like they’re dying? I’ve had migraines for 10 years and no one gives me a medal. Just saying.
Steve Phillips
November 21, 2025 AT 08:06Let’s be real-this is the most comprehensive lupus guide I’ve ever seen… but why is no one talking about the fact that 70% of lupus patients are women? And why are we still using 1980s treatment protocols? Anifrolumab? That’s a miracle drug. Why isn’t it first-line? Because Big Pharma doesn’t profit from a ‘cure’-they profit from lifelong maintenance. Wake up.
Rachel Puno
November 22, 2025 AT 05:04Just started hydroxychloroquine last month. I was skeptical. Now I’m walking my dog for 30 minutes every day. I have energy. I’m not cured-but I’m alive again. Thank you for the practical advice. This isn’t just medical info-it’s hope.
Clyde Verdin Jr
November 23, 2025 AT 03:07Wow. So basically, lupus is just a fancy word for ‘your immune system is broken.’ And the treatment? Take a pill you’ve never heard of, wear sunscreen like it’s your job, and pray you don’t get a kidney infection. Great. So we’re all just waiting to die slowly. Thanks for the pep talk, doc.