Most people think if your thyroid hormone levels are normal, you’re fine. But what if your TSH is high - and everything else looks okay? That’s subclinical hypothyroidism. It’s not the full-blown version where you feel exhausted, gain weight, and can’t stay warm. You might feel fine. Or maybe you just think you’re getting older. But here’s the real question: should you take medication for it?
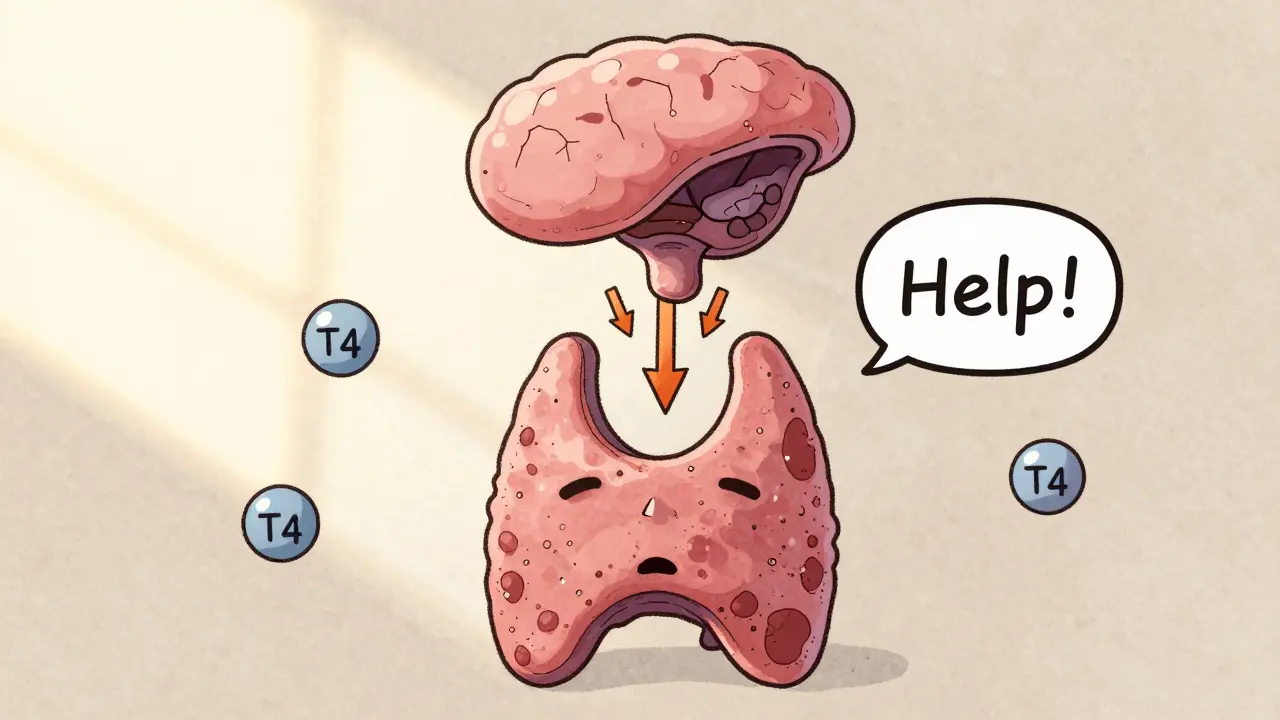
What Exactly Is Subclinical Hypothyroidism?
Subclinical hypothyroidism means your thyroid-stimulating hormone (TSH) is above the normal range, but your free T4 - the main active thyroid hormone - is still perfectly normal. It’s like your thyroid is whispering for help, but it’s not screaming yet. Your pituitary gland is pumping out more TSH because it’s trying to get your thyroid to work harder. But so far, your thyroid is keeping up.
This isn’t rare. About 1 in 5 adults in the U.S. have elevated TSH, especially as they get older. In people over 60, it’s even more common. But here’s the catch: not everyone with high TSH needs treatment. Some will never progress. Others might. And some will feel better on medication. Others won’t notice a thing.
When Is TSH Actually Too High?
The lab says your TSH is normal up to 4.5 or 5.0 mIU/L - but that’s where things get messy. That upper limit was set decades ago based on data that included people with undiagnosed thyroid problems. Newer studies suggest the true upper limit for healthy adults under 50 might be closer to 2.5 or 3.0 mIU/L. But most labs still use 4.5 or 5.0 as the cutoff.
So if your TSH is 5.2? That’s elevated. But is it a problem? The answer depends on three things: your age, your symptoms, and whether you have thyroid antibodies.
Thyroid Antibodies: The Hidden Clue
If you have thyroid peroxidase (TPO) antibodies, your immune system is already attacking your thyroid. That’s Hashimoto’s - the most common cause of hypothyroidism. If your TSH is high and your TPO antibodies are positive, your thyroid is likely on its way down. Studies show these patients have more than a 2 in 3 chance of developing full-blown hypothyroidism within four years if their TSH is above 8 mIU/L.
That’s why doctors who treat subclinical hypothyroidism closely look at antibody status. A TSH of 7.5 with positive antibodies? That’s a red flag. A TSH of 7.5 with negative antibodies? Much less concerning. Antibodies are the best predictor of what’s coming next.
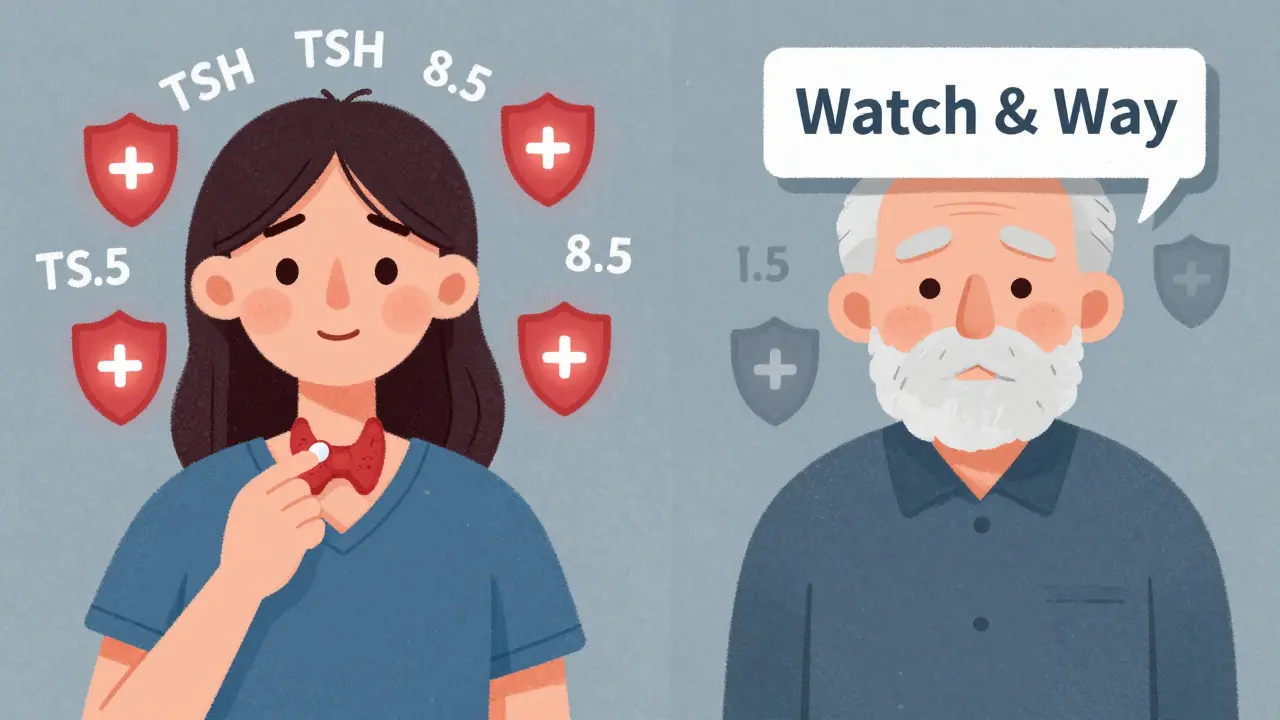
Age Matters - A Lot
If you’re 28 and your TSH is 8.1, your doctor might suggest starting a low dose of levothyroxine. If you’re 78 and your TSH is 8.1? They might say, “Let’s just watch it.”
Why? Because treating older adults with mild TSH elevation can be dangerous. A 2021 analysis found that people over 65 with TSH under 10 mIU/L who took thyroid medication had a 12% higher risk of dying from any cause. Why? Too much thyroid hormone can cause atrial fibrillation, bone loss, and muscle weakness - problems that are already common in older adults.
For younger people, the risks of not treating are bigger. Untreated subclinical hypothyroidism can raise LDL cholesterol, increase blood pressure, and raise your risk of heart disease over time. One study showed a 32% drop in fatigue and brain fog in people under 50 with TSH 7-10 mIU/L and positive antibodies after starting treatment.
Do Symptoms Even Matter?
You’re tired. Your skin is dry. You’re gaining weight. You feel down. You think it’s your thyroid. But here’s the truth: most people with subclinical hypothyroidism don’t have symptoms that are any worse than people with normal thyroid function.
A large 2017 trial called TRUST looked at 737 older adults with TSH between 4 and 10 mIU/L. Half got levothyroxine. Half got a placebo. After one year? No difference in energy, mood, or quality of life. Another study found that 30-40% of people who think their symptoms are from thyroid issues actually have them for other reasons - sleep apnea, depression, low vitamin D, or just aging.
But here’s the twist: some people do feel better. A lot of patients on forums like Reddit’s r/hypothyroid say their fatigue vanished after starting 25 mcg of levothyroxine. Their TSH was 8.5. Their antibodies were positive. They felt awful. And they felt better. So why doesn’t the science show it?
Because trials average out everyone. They don’t pick out the 15-20% who really benefit. If you’re young, have antibodies, and have clear symptoms - your experience matters. It’s not just in your head.
What Do the Guidelines Actually Say?
There’s no global agreement. Here’s what the major groups say:
- American Thyroid Association (ATA): Treat only if TSH is above 10 mIU/L.
- American Association of Clinical Endocrinologists (AACE): Consider treatment if TSH is above 7-8 mIU/L, especially with antibodies or symptoms.
- Endocrine Society: Treat TSH >10 mIU/L. Consider treatment for TSH 7-10 mIU/L if you’re young, have antibodies, or have heart disease risk.
- Royal Australian College of General Practitioners (RACGP): Don’t treat routinely for TSH 4-10 mIU/L.
- AAFP (American Academy of Family Physicians): Treat TSH >10 mIU/L or if TPO antibodies are positive.
That’s a lot of confusion. And it’s why two doctors can look at the same lab results and give completely different advice.
When Should You Start Medication?
Here’s a simple decision tree based on current evidence:
- TSH >10 mIU/L? Start levothyroxine. The benefit is clear.
- TSH 7-10 mIU/L and TPO antibodies positive? Strongly consider starting. You’re likely to progress. Symptoms? Even more reason.
- TSH 7-10 mIU/L and TPO antibodies negative? Monitor. Repeat TSH in 6 months. No need to rush into medication.
- TSH 5-7 mIU/L? Watch and wait. Only treat if you have strong symptoms, high cholesterol, or are planning pregnancy.
- Over 65 with TSH <10 mIU/L? Don’t treat unless you have clear signs of heart disease or severe symptoms.
Starting dose? Usually 25-50 mcg of levothyroxine. Don’t go higher right away. Older adults and those with heart disease should start at 25 mcg. Recheck TSH in 6-8 weeks. Adjust slowly. The goal isn’t to make TSH zero - it’s to bring it back into the normal range, usually between 0.5 and 4.0 mIU/L.
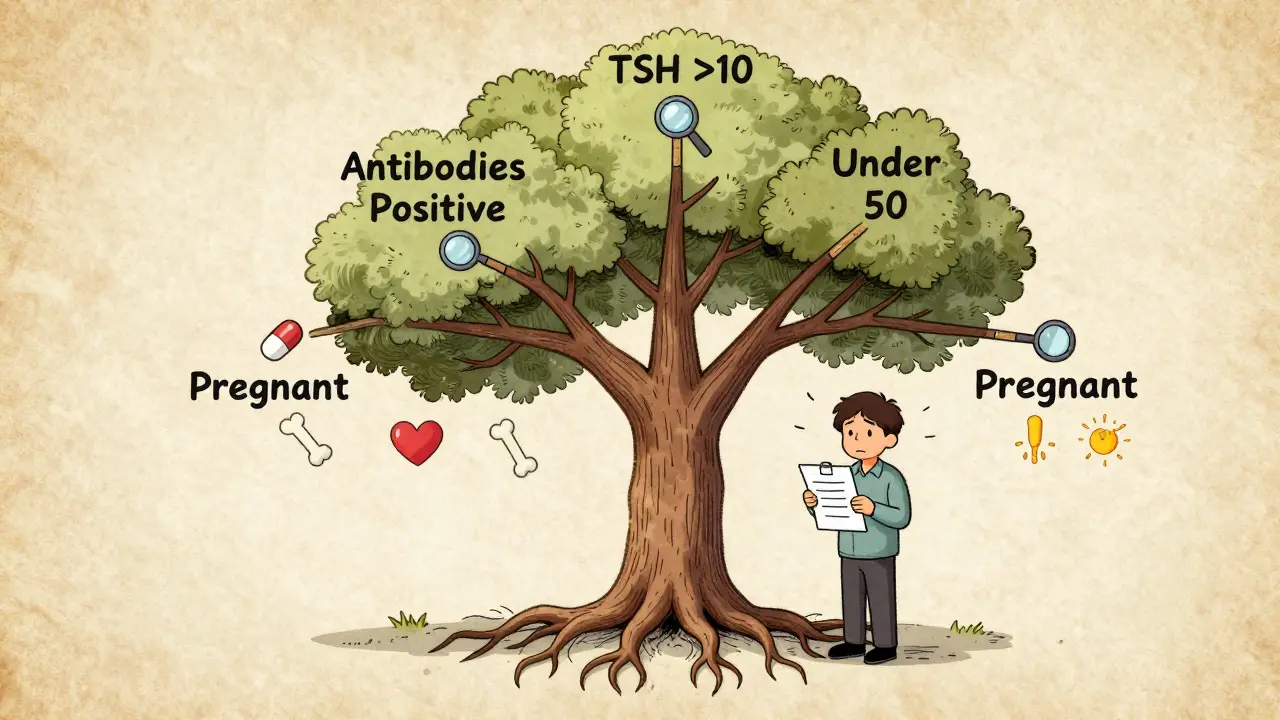
What About Pregnancy?
If you’re trying to get pregnant or already pregnant, treat subclinical hypothyroidism - even if your TSH is only 4.5. Thyroid hormone is critical for early brain development in the fetus. The American Society for Reproductive Medicine recommends keeping TSH under 2.5 during preconception and first trimester. If you’re pregnant and your TSH is above 4.0, start levothyroxine immediately.
What You Should Do Next
If your TSH is high:
- Get your TPO antibodies tested - this is non-negotiable.
- Check your cholesterol and blood pressure.
- Use a symptom checklist like the Thyroid Symptom Rating Scale - don’t rely on vague feelings.
- Don’t start medication without a plan. Recheck TSH in 6-8 weeks after starting.
- If you’re over 65, ask your doctor: “What’s the risk of treating vs. not treating?”
And if your doctor says, “Just monitor,” that’s okay - if you’re young, antibody-negative, and feel fine. But if you’re under 50, have antibodies, and feel awful? Push for a trial. You have nothing to lose and everything to gain.
The Bottom Line
Subclinical hypothyroidism isn’t a disease you can treat with a one-size-fits-all rule. It’s a warning sign - and how you respond depends on your age, your antibodies, your symptoms, and your risk for heart disease. For some, treatment prevents bigger problems. For others, it’s just a pill they don’t need.
Don’t let a number on a lab report decide your health. Let your whole picture - your body, your history, your life - guide the decision. And if you’re unsure? Get a second opinion from an endocrinologist. This isn’t about being overly cautious. It’s about being smart.
Is subclinical hypothyroidism the same as Hashimoto’s?
No. Subclinical hypothyroidism means your TSH is high but your thyroid hormone levels are normal. Hashimoto’s is an autoimmune disease where your immune system attacks your thyroid. Many people with subclinical hypothyroidism have Hashimoto’s - especially if they test positive for TPO antibodies. But you can have subclinical hypothyroidism without Hashimoto’s, and you can have Hashimoto’s without elevated TSH - especially in the early stages.
Can I just take iodine or supplements instead of levothyroxine?
No. Iodine supplements won’t help if your thyroid is being attacked by your immune system (Hashimoto’s). In fact, too much iodine can make it worse. Selenium might help reduce antibody levels slightly, but it won’t fix high TSH. Levothyroxine replaces the hormone your thyroid isn’t making enough of. There’s no natural substitute that works as reliably.
How long do I need to take levothyroxine for subclinical hypothyroidism?
If you start treatment because your TSH is high and you have positive antibodies, you’ll likely need it for life. Thyroid damage from Hashimoto’s is usually permanent. But if your TSH was high due to stress, illness, or medication, and your antibodies are negative, your doctor might try stopping after 6-12 months to see if your thyroid recovers. This is rare, though.
Can high TSH cause weight gain?
Mildly elevated TSH alone doesn’t cause significant weight gain. People with overt hypothyroidism often gain 5-10 pounds due to fluid retention and slower metabolism. But in subclinical cases, weight gain is usually due to other factors - diet, sleep, stress, or lack of movement. Treating subclinical hypothyroidism rarely leads to major weight loss. Don’t start medication just to lose weight.
What if my TSH is normal but I still feel awful?
If your TSH and free T4 are normal, you don’t have hypothyroidism. Your symptoms are real - but they’re probably not from your thyroid. Look at sleep quality, stress levels, vitamin D, iron, B12, and mental health. Many people with fatigue, brain fog, or low mood have other causes. Don’t chase thyroid treatment if your labs are clean. You’ll waste time and money - and risk side effects.
What’s Next?
Research is moving fast. The SHINE trial, expected to finish in late 2024, will tell us whether treating subclinical hypothyroidism reduces heart attacks and strokes. Meanwhile, new tools are being developed to track TSH velocity - how fast your TSH is rising - which may be a better predictor of future problems than a single number.
For now, the safest approach is to avoid treating unless the evidence clearly points to benefit. But if you’re young, have antibodies, feel unwell, and your TSH is above 7 - don’t wait. Your future self might thank you.

caroline hernandez
February 2, 2026 AT 16:45Subclinical hypothyroidism is such a gray zone - TSH above 4.5 doesn’t automatically mean pathology, but when you’ve got positive TPO antibodies and symptoms like brain fog or elevated LDL, you’re looking at early Hashimoto’s in motion. The pituitary is screaming for help, and ignoring it is like ignoring a check engine light because the car still drives. Treatment isn’t about ‘fixing’ something broken - it’s about halting progression. I’ve seen patients with TSH 8.2 and negative antibodies stay stable for years, while others with TSH 6.1 and positive antibodies crash into overt hypothyroidism in 18 months. Antibody status is the real prognostic marker, not the TSH number alone.
Jhoantan Moreira
February 2, 2026 AT 22:42Really appreciate this breakdown 🙏 I’ve been TSH 6.8 for 3 years, antibodies positive, zero symptoms - and my doc said ‘wait and see.’ Now I’m wondering if I’m just lucky or if I’m silently harming my heart. Maybe I’ll get a lipid panel done this week. Thanks for the clarity!
Joseph Cooksey
February 4, 2026 AT 12:18Let’s be real - the entire endocrine establishment is a profit-driven mess. Labs set the ‘normal’ TSH range at 5.0 because if they lowered it to 2.5, half the population would be ‘hypothyroid’ and on levothyroxine. Pharma loves that. Meanwhile, real people suffer from fatigue, weight gain, and depression while being told it’s ‘just stress’ or ‘aging.’ The TRUST trial? Flawed. They used a one-size-fits-all 50 mcg dose for elderly patients who needed 12.5 mcg. Of course they saw no benefit - you’re giving a diabetic insulin and then blaming them for hypoglycemia. The data is rigged to protect the status quo. If you’re under 50, have antibodies, and feel like crap - start low and go slow. Your body isn’t lying. The guidelines are.
Justin Fauth
February 4, 2026 AT 12:36Why are we letting bureaucrats and pharmaceutical reps decide what’s normal for our bodies? In my dad’s time, TSH over 4.0 was treated. Now? We’re told to wait until it hits 10? That’s not medicine - that’s negligence wrapped in a white coat. I’m 32, TSH 7.3, antibodies up, and I had zero energy. Took 25 mcg. Felt like I’d been asleep for 10 years and just woke up. My cholesterol dropped 40 points. This isn’t anecdotal - it’s biology. Stop waiting for permission to feel human again.
Meenal Khurana
February 6, 2026 AT 09:24TSH 7.1, antibodies positive. Started 12.5 mcg. Better in 2 weeks. No drama.
Joy Johnston
February 8, 2026 AT 03:51While the evidence for treating subclinical hypothyroidism remains nuanced, it is imperative to consider individual risk stratification. Patients with elevated thyroid peroxidase antibodies, particularly those under the age of 50, demonstrate a statistically significant increased likelihood of progression to overt hypothyroidism. Furthermore, the presence of dyslipidemia or cardiovascular risk factors may justify earlier intervention, given the potential for subclinical thyroid dysfunction to exacerbate atherosclerotic burden. A cautious, individualized approach - rather than a rigid TSH threshold - aligns with the principles of precision medicine.
Sherman Lee
February 9, 2026 AT 01:24Did you know the FDA approved levothyroxine based on a 1950s study with 12 patients? And now we’re told to ignore it unless TSH hits 10? 🤡 The real agenda? Big Pharma doesn’t want you feeling better on $5/month. They want you on 12 different meds for ‘symptoms’ they created. Also - did you know TSH is regulated by the hypothalamus, not the thyroid? They never teach that in med school. Your pituitary is the boss. If it’s screaming, your thyroid is trying. Stop listening to guidelines written by people who’ve never had a thyroid problem. I’ve seen people cured by just fixing their gut. Thyroid meds are a band-aid on a bullet wound.
Amit Jain
February 9, 2026 AT 05:36My mom had TSH 8.5, no symptoms. Doctor said no medicine. One year later, she felt tired, gained weight. Started medicine. Now she’s fine. So if you have high TSH, don’t wait. Check antibodies. If positive, treat early.
Keith Harris
February 10, 2026 AT 08:06Oh wow, another ‘trust your doctor’ post. How cute. You think the American Thyroid Association gives a damn about your fatigue? They’re funded by drug companies that sell $120/month thyroid meds. Meanwhile, your real issue is mold toxicity, Lyme, or gut dysbiosis - but nope, let’s just throw levothyroxine at it and call it a day. I’ve seen 30 people on T4 who felt worse until they went T3-only. But hey, let’s keep pretending TSH is the whole story. 🤷♂️
Kunal Kaushik
February 11, 2026 AT 18:59Thanks for writing this. I’ve been TSH 6.2 for 2 years, antibodies positive, but no symptoms. Still, I’m scared to wait. I feel like I’m walking a tightrope between ‘overmedicating’ and ‘ignoring a ticking time bomb.’
Mandy Vodak-Marotta
February 11, 2026 AT 22:16I was diagnosed with subclinical hypothyroidism at 29. TSH 8.1, TPO antibodies through the roof. My doctor said ‘wait till it hits 10.’ I waited 8 months. By then, I couldn’t get out of bed. My hair was falling out. I cried every morning. Started 25 mcg. Within 3 weeks, I could run again. I’m not ‘cured’ - but I’m alive. People who say ‘it’s all in your head’ haven’t lived it. Don’t wait. Don’t listen to guidelines that don’t care if you’re depressed, tired, or losing your hair. Your body is trying to tell you something. Listen.
Nathan King
February 12, 2026 AT 09:25The clinical ambiguity surrounding subclinical hypothyroidism reflects the broader epistemological limitations of evidence-based medicine when applied to heterogeneous populations. While population-level trials such as TRUST provide valuable insights, they are inherently reductionist and fail to account for individual phenotypic variability. A TSH threshold of 10 mIU/L, while statistically convenient, is not a biological imperative. The concept of ‘normal’ thyroid function must be reconceptualized through the lens of personalized physiology rather than population norms.
Harriot Rockey
February 13, 2026 AT 23:41Hey - if you’re reading this and you’re scared about your TSH? You’re not alone. I was there. I had TSH 7.9, antibodies positive, and I felt like a ghost. I didn’t want to be on meds… but I didn’t want to keep feeling like I was underwater either. I started with 12.5 mcg. Took 2 weeks. I cried because I remembered what it felt like to wake up excited. You’re not crazy. You’re not ‘just tired.’ Your body is asking for help. And it’s okay to say yes. 💛
rahulkumar maurya
February 15, 2026 AT 02:44Most people don’t realize that TSH is not a hormone - it’s a signal. The thyroid doesn’t produce TSH; the pituitary does. So when TSH is high, it means the brain thinks the thyroid is underperforming. But why? Maybe it’s inflammation. Maybe it’s selenium deficiency. Maybe it’s cortisol dysregulation. Levothyroxine doesn’t fix the root cause - it just masks the symptom. Real medicine asks ‘why?’ - not ‘how much T4?’
Justin Fauth
February 16, 2026 AT 16:28And yet, the people who say ‘it’s just inflammation’ or ‘fix your gut’ are the same ones who told me to take turmeric and stop eating gluten. I did. I still had a TSH of 8.1. I still couldn’t think straight. I still needed the med. You can’t ‘eat your way out’ of an autoimmune attack on your thyroid. That’s not nutrition - that’s denial.