When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how does the FDA make sure that generic drug stays safe and effective for months-or even years-after it leaves the factory? The answer lies in stability testing, one of the most critical, yet least understood, parts of getting a generic drug approved.
Why Stability Testing Matters for Generics
Stability testing isn’t just paperwork. It’s science that proves your medicine won’t fall apart on the shelf. If a tablet loses potency, a liquid turns cloudy, or a capsule leaks, the drug might not work-or worse, it could harm you. The FDA requires every generic drug to prove it behaves the same as the brand-name version over time, under real-world conditions like heat, humidity, and light.Generic manufacturers don’t get a free pass. Even though they copy an existing drug, they must test their own batches. Why? Because changing the manufacturing process, ingredients, or packaging-even slightly-can affect how the drug holds up. A generic made in India might use different fillers or a different bottle than the U.S. brand. Stability testing catches those differences before the drug reaches patients.
What the FDA Actually Requires
The FDA’s rules for stability testing come from two main sources: the ICH Q1A(R2) guidelines and their own 2018 Q&A document for ANDA submissions. Here’s what you need to know:- You must test at least three production-scale batches of the drug. These aren’t lab samples-they’re made using the same equipment and process you’ll use to supply the market.
- Each batch must be packaged in the exact same container and closure system you plan to sell. No shortcuts.
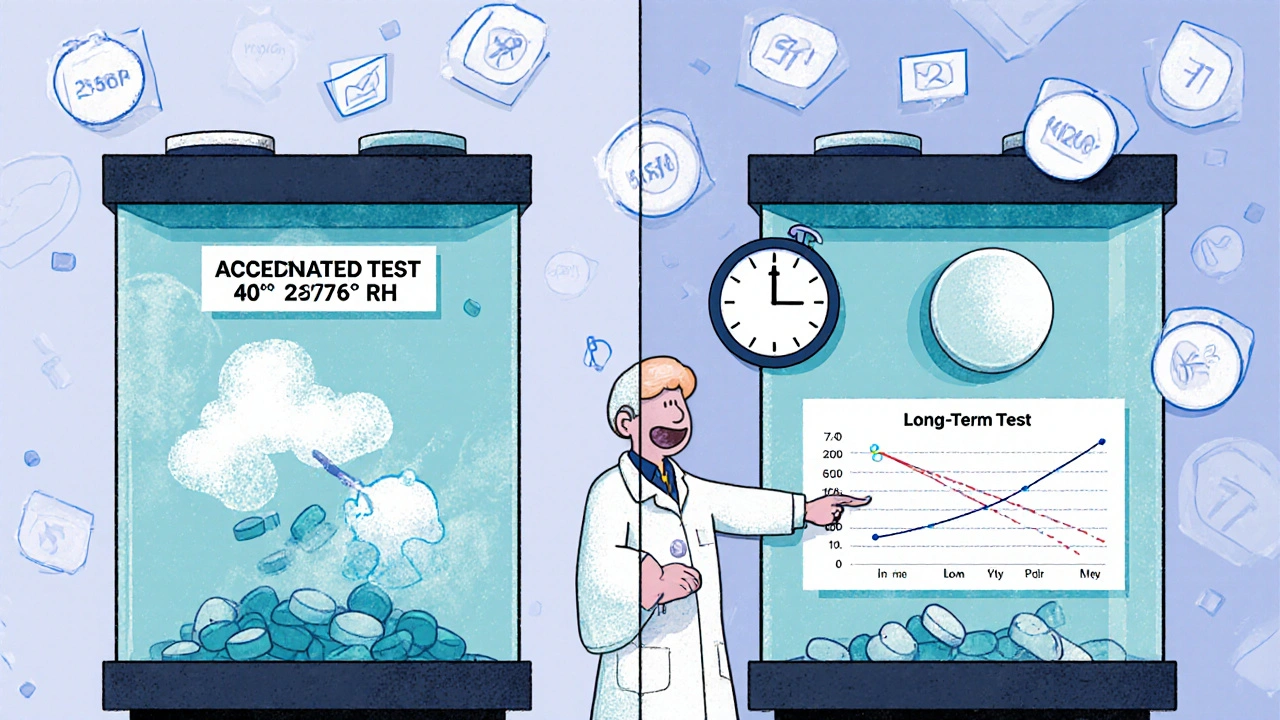
- You need both long-term and accelerated testing. Long-term means storing samples at 25°C ± 2°C and 60% ± 5% RH for at least 12 months. Accelerated testing is harsher: 40°C ± 2°C and 75% ± 5% RH for 6 months.
- Testing frequency? Every 3 months for the first year, every 6 months for the second year, and once a year after that.
- You must test for physical changes (color, texture), chemical changes (potency, impurities), biological changes (microbial growth), and functionality (does the inhaler still spray properly?).
The FDA doesn’t accept guesses. You need hard data. If your tablet drops below 90% potency before the expiration date, your application gets rejected. Period.
How Generics Differ from Brand-Name Drugs in Testing
You might think generics get a lighter load because they’re copying something already approved. But that’s not how it works.Brand-name companies spend years building stability data from scratch. They test dozens of formulations, run forced degradation studies to see how the drug breaks down, and map out every possible impurity. Generics don’t need to do all that. They can reference the brand’s data to understand degradation pathways-but they still must run their own tests on their product.
Here’s the key difference: brand-name companies prove their drug works. Generics prove their version matches it. That means the FDA compares your stability data directly to the reference listed drug (RLD). If your tablet degrades faster, or forms different impurities, you’re not approved.
Common Reasons Generic Applications Get Rejected
Stability testing is the #1 reason generic applications get turned down. According to FDA data from 2019, nearly 35% of Complete Response Letters (CRLs) were due to stability issues. Here’s what goes wrong most often:- Missing or vague protocols: If your test plan doesn’t say exactly how you’ll measure potency or impurities, the FDA will reject it. You need to cite USP chapters like <1151> and <1010>.
- Not enough data points: Testing only at 0 and 6 months? Not enough. You need at least 6 months of long-term data and 6 months of accelerated data for review.
- Improper storage conditions: Stability chambers must hold 25°C ± 2°C and 60% RH. A 3°C spike for a week can invalidate your whole study. In 2022, 18.4% of data failures came from temperature excursions.
- Unvalidated test methods: If your HPLC method can’t detect a new impurity, it’s useless. The FDA requires full method validation before you start testing.
- Wrong container: Testing in glass vials but selling in plastic bottles? That’s a red flag. Packaging affects moisture and oxygen exposure.
One manufacturer lost approval because their stability chamber logged a 4.7°C spike three times a month. The FDA didn’t care if the drug was fine-they cared that the data couldn’t be trusted.
How Manufacturers Are Adapting
To avoid rejection, top generic companies are investing in better systems:- Automated monitoring: 78.4% of top 25 generic makers now use real-time sensors to track temperature and humidity. Alerts pop up if conditions drift.
- Bracketing and matrixing: Instead of testing every strength and size, companies test only the extremes (highest and lowest doses) and use statistical models to cover the rest. This saves time and money-if the FDA approves the design.
- Pre-submission meetings: Companies now schedule meetings with the FDA before submitting. This cuts deficiency rates by over 40%.
- Blockchain pilots: Starting in 2025, the FDA is testing blockchain to lock stability data so it can’t be altered. Think of it like a tamper-proof logbook.
These aren’t luxuries-they’re necessities. With 92.7% of stability-related deficiencies coming from generic applications (vs. 78.4% from brand-name), the bar is higher for generics.
What’s Changing in 2025 and Beyond
The FDA isn’t slowing down. New rules are coming:- 24-month long-term data: Starting in 2025, new ANDAs will need 24 months of real-time stability data instead of 12. This means longer wait times for approvals.
- Quality by Design (QbD): You can’t just test at the end. You must design stability into the product from the start-using risk assessments, process controls, and science-based decisions.
- Nanomaterials and biosimilars: New drugs using nanoparticles or biologics need extra stability tests. Biosimilars now require 12 months of comparative data against the reference product.
- Climate zones: The ICH is updating guidelines to require testing under conditions that match where the drug will be sold-like tropical climates in Southeast Asia or arid regions in the Middle East.
These changes aren’t just about safety-they’re about global access. A drug that works in Ohio must also work in Nigeria. That’s why the FDA is pushing for more realistic, global standards.
The Cost of Getting It Right
Stability testing isn’t cheap. On average, it costs $487,500 per generic drug application-about 18.7% of total development costs. For a company submitting 10 applications a year, that’s nearly $5 million just on stability.Indian manufacturers, who supply 40% of U.S. generics, face the toughest hurdles. In 2022, they accounted for 63% of all stability-related rejections. Why? Smaller labs, less automation, and pressure to cut costs. But the FDA doesn’t make exceptions. If your data isn’t solid, you don’t get approved.
Meanwhile, the U.S. generic market is worth $127 billion. Companies can’t afford to fail. The ones investing in better systems are winning. The ones cutting corners? They’re stuck in review limbo.
What You Should Know as a Patient
You don’t need to understand chromatography or humidity chambers. But you should know this: every generic you take has been tested to the same standard as the brand. The FDA doesn’t allow shortcuts. If your generic looks different, tastes different, or comes in a different bottle, it’s still held to the same quality bar.Expiration dates aren’t guesses. They’re backed by real data. If your pills are past their date, don’t take them. The FDA doesn’t recommend using expired meds-even generics-because stability can’t be guaranteed after that point.
And if you ever wonder why a generic takes longer to hit the market? Stability testing is often the bottleneck. It’s not about profit-it’s about proof.
Do generic drugs need the same stability testing as brand-name drugs?
Yes. Both must follow the same ICH Q1A(R2) guidelines. Brand-name companies build stability data from scratch. Generics use the brand’s data as a reference but must still test their own batches under identical conditions to prove equivalence. The FDA compares the stability profiles directly.
How long does stability testing take before a generic drug is approved?
You need at least 6 months of accelerated data and 6 months of long-term data to submit an ANDA. But full approval often requires 12 months of real-time data. With the new 2025 requirements, applicants will need 24 months of long-term data, meaning approval timelines could extend by 6-12 months.
What happens if a generic drug fails stability testing?
The FDA issues a Complete Response Letter (CRL), rejecting the application. The manufacturer must fix the issue-usually by running more tests, improving packaging, or adjusting the formulation-and resubmit. This can delay market entry by 6 months to over a year.
Can I trust the expiration date on a generic drug?
Absolutely. The expiration date is based on real-time stability data showing the drug remains within strict quality standards. The FDA requires this data for every approved generic. If the drug degrades before the date, it won’t be approved.
Why do some generic drugs look different from the brand?
Generics can use different inactive ingredients (like fillers or dyes) and different packaging, as long as they don’t affect stability or absorption. The FDA requires proof that these differences don’t change how the drug performs over time. That’s why stability testing is so important-it ensures the look doesn’t affect the performance.
Are there any shortcuts to stability testing for well-known generic drugs?
No formal shortcuts exist. Even for drugs with decades of use, the FDA requires new stability data for each manufacturer’s version. However, companies can use bracketing (testing only the highest and lowest strengths) or matrixing (testing selected time points) to reduce the number of samples-only if scientifically justified and approved by the FDA.
What Comes Next
The future of generic drug approval is clearer but tougher. The FDA is moving toward more science-based, data-driven decisions. Automation, blockchain, and global standards are becoming the norm. Manufacturers who treat stability testing as a compliance chore will keep getting rejected. Those who treat it as core to product quality will thrive.For patients, this means more confidence in generics. For the industry, it means higher costs and longer timelines. But in the end, it’s not about regulation for regulation’s sake. It’s about making sure every pill you take-no matter the price-still works when you need it.

Kimberley Chronicle
November 25, 2025 AT 15:53Stability testing for generics is such a critical but invisible pillar of pharmaceutical safety. The ICH Q1A(R2) framework isn’t just bureaucratic red tape-it’s the scientific backbone ensuring that a tablet manufactured in Chennai performs identically to one made in New Jersey. The real win? The FDA’s insistence on comparative data against the RLD. That’s not laziness-it’s precision. Without this, we’d be flying blind on bioequivalence.
And let’s talk about packaging. A plastic bottle vs. glass isn’t just a cost decision-it’s a diffusion pathway. Moisture ingress can hydrolyze esters, oxidize phenols, and degrade peptides. If your container closure system isn’t validated for the drug’s physicochemical profile, you’re not just risking efficacy-you’re risking patient harm. This isn’t theory. It’s pharmacokinetics in action.
Shirou Spade
November 25, 2025 AT 21:25It’s funny how we treat medicine like a product when it’s really a covenant between science and suffering. The generic manufacturer doesn’t just copy a molecule-they copy a promise. That promise is sealed not by marketing, but by stability chambers humming at 25°C and 60% RH. Every data point is a silent vow: ‘I will not fail you.’
And yet, we reduce this to price tags. We cheer the 90% cost savings but forget the 12-month studies, the validated HPLC methods, the technicians logging temperatures at 3 a.m. The real miracle isn’t that generics exist-it’s that they work, reliably, every single time.
Lisa Odence
November 26, 2025 AT 04:53OMG I JUST REALIZED WHY MY GENERIC IBUPROFEN TASTES LIKE PLASTIC 😱
IT’S BECAUSE THE PACKAGING ISN’T BARRIER-VALIDATED!!
THE FDA REQUIRES EXACT SAME CLOSURE SYSTEM AS RLD-SO IF YOURS IS PLASTIC AND THE BRAND IS GLASS, THAT’S A VIOLATION!!
AND DON’T EVEN GET ME STARTED ON TEMPERATURE EXCURSIONS!! 4.7°C SPIKE?? THAT’S NOT A FLUCTUATION-THAT’S A SCANDAL!!
WE NEED BLOCKCHAIN FOR STABILITY DATA NOW!! 🚨💊🔥
PS: I WORK IN PHARMA QUALITY AND THIS IS MY DAY JOB. I’M NOT JOKING. I’VE SEEN CRLs. THEY’RE TERRIFYING.
Ellen Sales
November 26, 2025 AT 19:17Let me just say-this is why I hate how people dismiss generics. They think it’s ‘the same drug’ so it must be ‘the same everything.’ But no. It’s the same active ingredient. The rest? Fillers. Binders. Coatings. Packaging. Manufacturing environment. All of it matters. And if you think the FDA lets someone slap a generic label on a pill that’s been sitting in a warehouse in Mumbai without controlled conditions-you’re delusional.
I’ve seen labs where the stability chamber was unplugged for three days because the intern forgot to pay the electric bill. That’s not negligence-it’s criminal. And the FDA catches it. Every time. Because they don’t trust humans. They trust data. And that’s why I sleep better at night knowing my generic metoprolol won’t turn into a chemical grenade.
giselle kate
November 27, 2025 AT 12:21India’s generic industry is a joke. They cut corners, hire untrained technicians, and use expired reagents just to make a buck. The FDA rejects 63% of their submissions because they’re lazy and greedy. And now they want to sell us pills that might degrade in a hot car? No thanks. We need to ban Indian generics. Build our own. Make America safe again. This isn’t about medicine-it’s about sovereignty. The FDA is doing its job. Why aren’t we?
Roscoe Howard
November 28, 2025 AT 02:08It is important to note that the regulatory framework governing generic drug stability is not merely a set of guidelines but a codified epistemological requirement for evidentiary validity. The requirement for three production-scale batches, each packaged in the identical container-closure system intended for commercial distribution, constitutes a necessary condition for inferential generalizability. Without this, the data cannot be extrapolated to the population of marketed units. Furthermore, the temporal resolution of testing-quarterly for the first year-is not arbitrary; it is derived from kinetic degradation models validated through accelerated aging protocols. To suggest otherwise is to misunderstand the very nature of pharmaceutical science.
Leisha Haynes
November 29, 2025 AT 16:22Y’all act like the FDA is some superhero saving us from evil generic companies
nah
the FDA is just the guy who shows up after the house burns down and says ‘well you shouldn’t have used cardboard for insulation’
the real problem? The system rewards speed over safety. Companies rush to submit because the market waits. The FDA says ‘no’ because they have to. But nobody’s fixing the broken incentives.
and yes i’ve seen a lab where the stability data was backfilled from a spreadsheet. it was real. and yes they got approved. eventually.
Arup Kuri
November 30, 2025 AT 16:53they’re lying about the testing. the real reason generics are cheaper is because the FDA lets them skip half the tests. the 63% rejection rate? that’s just the ones they caught. the rest are on shelves. you think they test every batch? no. they test one batch and lie about the rest. and the blockchain thing? that’s just a distraction. the government wants to track you not your pills. trust me i know.
Elise Lakey
December 2, 2025 AT 14:33Thank you for writing this. I’ve been on a generic blood pressure med for years and never thought about how it’s tested. The fact that it’s held to the same standard as brand-name drugs is actually really comforting. I’m glad the FDA doesn’t cut corners-even if it makes things slower. Safety over speed, always.
Timothy Sadleir
December 2, 2025 AT 16:45The notion that generics are somehow ‘lesser’ is a fallacy born of ignorance. The regulatory equivalence paradigm, as codified under ANDA, does not permit inferiority. It demands congruence. The requirement for comparative stability profiles ensures that the pharmacokinetic and pharmacodynamic behavior of the generic is not merely similar-it is statistically indistinguishable. The fact that some manufacturers fail is not a flaw in the system; it is evidence of its rigor. To demand less would be to abandon the very foundation of evidence-based medicine.
Agastya Shukla
December 4, 2025 AT 05:09Bracketing and matrixing are brilliant-when done right. I’ve worked on a project where we tested only the highest and lowest strengths of a multi-strength tablet series. Used QbD principles to model degradation kinetics across the range. FDA approved it in one round. Saved $200K in testing costs. But here’s the catch: you need to submit the statistical model, the justification, the stability-indicating method validation data, and a risk assessment. No hand-waving. It’s not a shortcut-it’s smart science. Most companies don’t have the expertise to pull it off. That’s why they fail.
Josh Zubkoff
December 4, 2025 AT 16:40Okay so let me get this straight-after spending $500K on stability testing, the FDA can still say ‘no’ because your chamber had a 4.7°C spike three times a month?
That’s not regulation. That’s performance art.
Who decided that a single temperature fluctuation invalidates an entire year of data? Some guy in a suit who’s never seen a stability chamber? The system is broken. It punishes minor deviations while letting systemic fraud slide. And don’t even get me started on how the big pharma companies own the reference listed drugs. It’s a rigged game.
Also-blockchain? Really? We’re putting blockchain on pills now? Next they’ll be NFTing expiration dates.
Karen Willie
December 6, 2025 AT 08:22This is the quiet heroism of generic manufacturing. No headlines. No press releases. Just scientists in labs, running HPLC runs at midnight, logging humidity, double-checking batch records. They don’t get praised. But every time you pick up a $4 pill and it works exactly like the $100 one-it’s because of them.
Let’s not forget: the real cost isn’t in the testing. It’s in the patience. The waiting. The second chances. The resubmissions. The hope that next time, it’ll pass.
Thank you to everyone who does this work.