When your heart arteries are clogged, you have two main options: PCI or CABG
If you’ve been told you need revascularization for coronary artery disease, you’re probably facing a big decision. Two procedures dominate the conversation: PCI (Percutaneous Coronary Intervention) and CABG (Coronary Artery Bypass Grafting). One is a quick catheter procedure. The other is open-heart surgery. Both fix blocked arteries. But they’re not interchangeable. Choosing the wrong one can mean more chest pain, repeat procedures, or even a higher risk of death.
There’s no one-size-fits-all answer. Your age, diabetes status, how many arteries are blocked, and even which artery is most affected all matter. The best choice isn’t determined by what’s trendy or what’s cheaper-it’s based on hard data from large clinical trials and your unique anatomy.
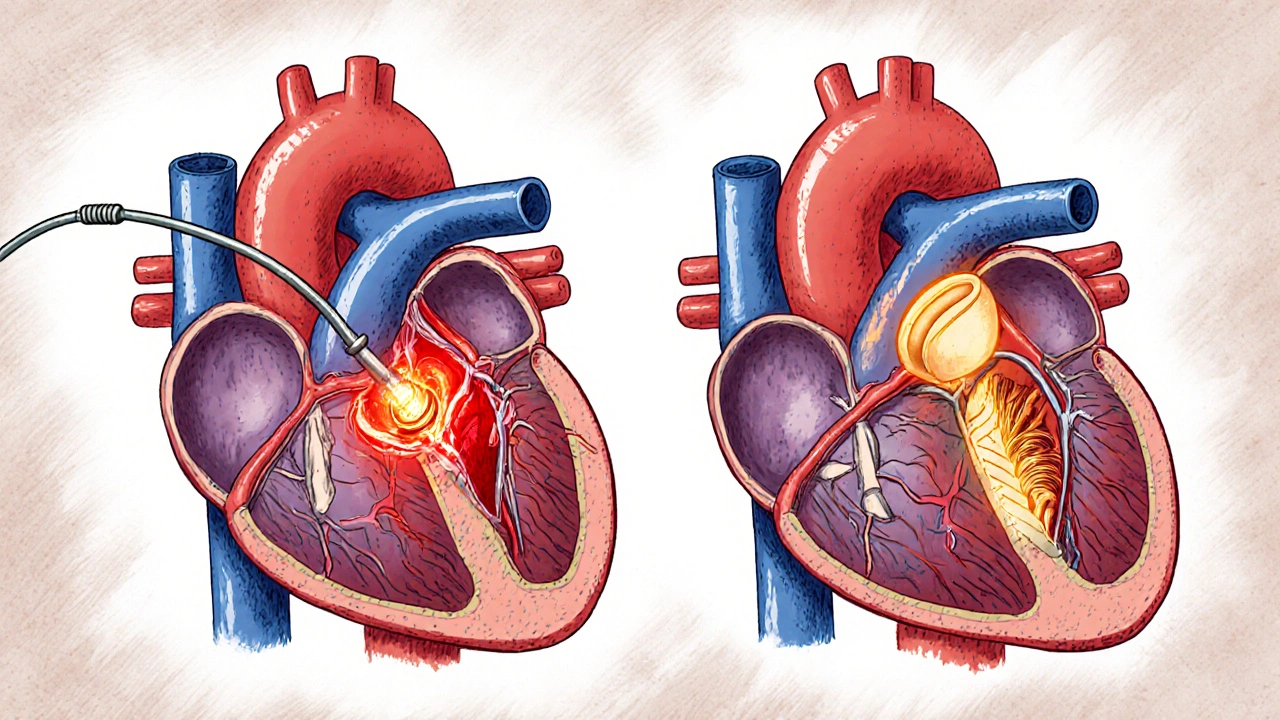
What is PCI? A stent procedure done through a wrist or groin
PCI is a minimally invasive procedure where a thin tube (catheter) is threaded from your wrist or groin up to your heart. A tiny balloon is inflated to open the blocked artery, and a metal mesh tube called a stent is left behind to keep it open. Most stents today are drug-eluting, meaning they slowly release medicine to prevent the artery from clogging again.
The whole thing usually takes 1 to 2 hours. You’re awake but sedated. Most people go home the next day. Recovery is fast: many are back to light work in 3 to 5 days. That’s the big appeal. No large incision. No weeks of healing.
But PCI has limits. It works best on single or simple blockages. If you have three blocked arteries, or if the blockage is in the main left artery (left main), PCI becomes riskier. Even with modern stents, about 5 to 10% of patients need another procedure within five years. That’s because the stent can re-narrow, or new blockages can form nearby.
Studies show PCI reduces chest pain well and improves quality of life in the short term. But for complex disease, it doesn’t lower the risk of heart attack or death as much as surgery.
What is CABG? Open-heart surgery that reroutes blood flow
CABG is open-heart surgery. Surgeons take a healthy blood vessel-usually from your chest wall (internal mammary artery), leg (saphenous vein), or arm (radial artery)-and graft it around the blocked section of your coronary artery. Think of it like building a detour for blood to flow past the obstruction.
The surgery takes 3 to 6 hours. You’re under full anesthesia. Recovery is longer: 5 to 7 days in the hospital, and 6 to 8 weeks before you feel like yourself again. You’ll have a long scar down your chest. Some people feel sternal pain for months.
But here’s the trade-off: CABG lasts longer. Arterial grafts (from your chest) stay open in 85 to 90% of cases after 10 years. Vein grafts are less durable, around 60 to 70%. That’s why surgeons prefer arterial grafts when possible.
CABG is more than just a bypass. It treats all the major blockages at once. That’s why it’s better for patients with multiple blocked arteries, especially if the left anterior descending (LAD) artery is involved. It’s also the gold standard for people with diabetes.
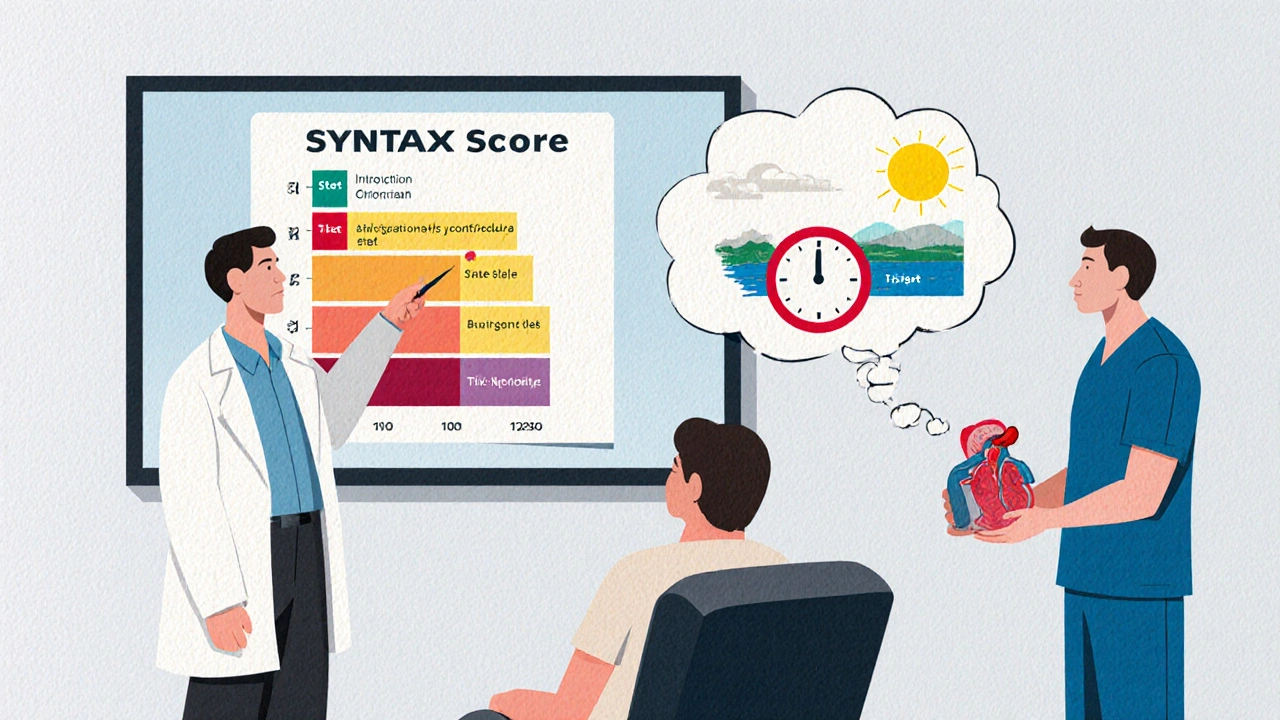
The SYNTAX score: How doctors decide between stent and bypass
Doctors don’t guess which procedure is better. They use a tool called the SYNTAX score. It’s a detailed analysis of your coronary angiogram that rates how complex your blockages are. The higher the score, the more complicated your disease.
- Score under 22: PCI is usually preferred
- Score between 22 and 32: Heart team discussion needed
- Score over 32: CABG is strongly recommended
This isn’t just theory. The SYNTAX trial (2009) showed that for patients with scores above 32, CABG cut major heart events by nearly half compared to PCI. Repeat procedures dropped from 16% to 7%.
But complexity isn’t everything. If you have diabetes, even a moderate SYNTAX score (say, 25) still points toward CABG. The FREEDOM trial proved that. Diabetics who got PCI had a 64% higher risk of death over five years than those who got bypass surgery.
For left main disease (a blockage in the main artery feeding the left side of the heart), the EXCEL and BEST trials showed similar survival rates between PCI and CABG at 3 years. But by year 5, CABG started pulling ahead. Why? Fewer repeat procedures. Fewer heart attacks. That’s the long-term advantage.
Survival, heart attacks, and repeat procedures: The hard numbers
Let’s look at what really matters: death, heart attack, and needing another procedure.
A 2019 meta-analysis of 11 major trials involving over 11,500 patients found:
- CABG reduced the risk of death by 18% over 5 years compared to PCI
- CABG cut heart attacks by 33%
- CABG reduced the need for repeat revascularization by more than half
But CABG comes with a trade-off: a slightly higher risk of stroke in the first 30 days. About 1.7% of CABG patients had a stroke versus 1% with PCI. That’s why doctors weigh brain health carefully-especially in older patients or those with a history of stroke.
For PCI, the big weakness is durability. Even with the best stents, 1 in 5 patients will need another procedure within five years. That’s not failure-it’s expected. But if you’re 55 and you get a stent, you might need three or four more over your lifetime. CABG patients rarely need a second surgery.
Diabetes changes everything
If you have diabetes, your arteries are more prone to rapid, widespread blockages. Your blood vessels heal poorly. That’s why PCI often falls short.
The FREEDOM trial was a landmark study. It followed 1,900 diabetic patients with multivessel disease. Half got PCI. Half got CABG. After five years:
- 16.4% of PCI patients died
- 10.0% of CABG patients died
That’s a 64% higher death rate for PCI. The difference was even clearer for heart attacks: 13.5% of PCI patients had one versus 5.9% of CABG patients.
Because of this, the American Heart Association and European Society of Cardiology both give CABG a Class IA recommendation-the strongest possible-for diabetic patients with multivessel disease. It’s not a suggestion. It’s a guideline backed by overwhelming evidence.
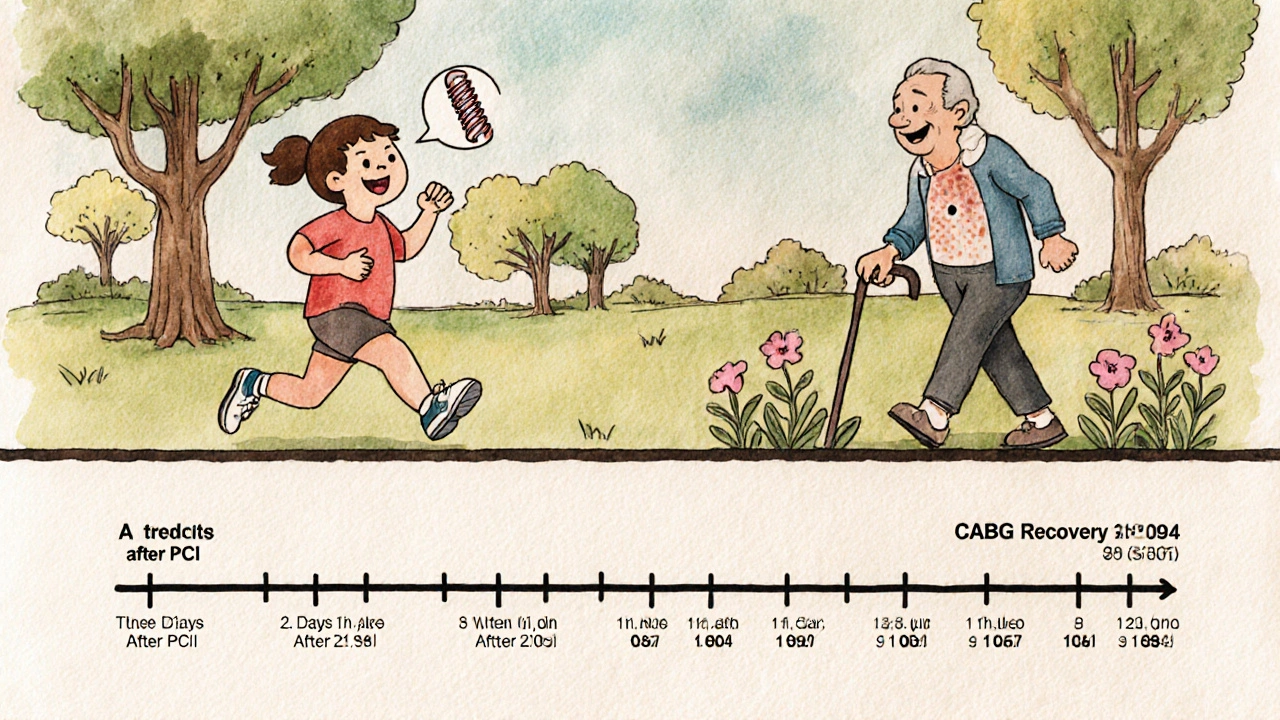
Recovery and quality of life: Fast return vs long-term relief
PCI wins on speed. CABG wins on sustainability.
At 30 days:
- 78% of PCI patients were back to normal daily activities
- Only 52% of CABG patients were
By six months, both groups were nearly equal. 94% of both had returned to work. But when you ask about chest pain and quality of life one year later, CABG patients report better outcomes. In the ROSETTA trial, 92% of CABG patients had complete relief from angina versus 85% of PCI patients.
Patients on Reddit often say the same thing: "PCI got me back to work fast, but I needed another stent after 18 months." Meanwhile, CABG patients say: "Six weeks of pain was worth it-I haven’t had chest pain in two years."
There’s also a psychological factor. People who get CABG often feel more confident knowing their arteries are bypassed with durable grafts. PCI patients sometimes live with the worry that another blockage is coming.
The heart team: Why two doctors should decide, not one
Guidelines now require a "heart team" for complex cases. That means an interventional cardiologist and a cardiac surgeon sit down together-with your records, your angiogram, your lab results-and decide as a team.
This isn’t bureaucracy. It’s necessary. Cardiologists are trained to do stents. Surgeons are trained to do bypasses. Left to their own devices, each might favor their own procedure. But when they collaborate, they focus on what’s best for you-not what’s easiest or most profitable.
High-volume centers (those doing over 400 PCIs or 200 CABGs a year) have better outcomes. Mortality for CABG drops from 3.2% in low-volume hospitals to 1.8% in high-volume ones. That’s why location matters. If you’re being offered a stent for complex disease, ask: "Has my case been reviewed by a cardiac surgeon?" If the answer is no, get a second opinion.
What’s new? Hybrid approaches and robotic surgery
Technology is changing the game. New stents are being developed with bioresorbable materials that dissolve after healing. Robotic-assisted CABG is becoming more common, allowing smaller incisions and faster recovery.
The most exciting development? Hybrid procedures. Imagine getting a minimally invasive bypass to the LAD artery (the most critical vessel) and a stent for the other blockages. This combines the durability of surgery with the speed of PCI. Early results are promising. Experts predict this approach will become standard for selected patients within the next five years.
One more thing: complete revascularization matters. If you have three blocked arteries, treating just one or two isn’t enough. The COMPLETE trial showed that treating all significant blockages-whether by stent or bypass-cuts future heart attacks and death by 25%.
Bottom line: How to choose
Here’s what you need to know:
- If you have simple blockages (one or two, low SYNTAX score), PCI is safe and effective.
- If you have diabetes and multiple blockages, CABG is the better choice for long-term survival.
- If you have left main disease and a high SYNTAX score (>32), CABG reduces heart attacks and repeat procedures.
- If you’re older, frail, or at high surgical risk, PCI might be the only safe option.
- Always insist on a heart team review. Don’t accept a decision made by one doctor alone.
Neither procedure is perfect. But the right one for you can mean years of pain-free life. The wrong one can mean repeated hospital visits, more stents, or worse.
Ask your doctor: "What’s my SYNTAX score?" "Am I diabetic?" "Is my LAD artery affected?" "Has my case been reviewed by a surgeon?" Those questions will guide you to the best outcome.

Jennifer Shannon
November 24, 2025 AT 04:14Suzan Wanjiru
November 24, 2025 AT 08:23Dalton Adams
November 26, 2025 AT 07:57Bryson Carroll
November 27, 2025 AT 17:40Henrik Stacke
November 28, 2025 AT 15:44Olanrewaju Jeph
November 30, 2025 AT 00:47Kane Ren
December 1, 2025 AT 08:16Karla Morales
December 3, 2025 AT 01:09Manjistha Roy
December 4, 2025 AT 06:31Jennifer Skolney
December 4, 2025 AT 21:10Charmaine Barcelon
December 6, 2025 AT 16:49JD Mette
December 6, 2025 AT 23:10Kezia Katherine Lewis
December 8, 2025 AT 09:43Javier Rain
December 9, 2025 AT 03:17