Why accurate cancer staging depends on the right imaging tool
Getting cancer staged right isn’t just a technical detail-it changes everything. A misread scan can mean the difference between starting chemotherapy too early, missing a hidden spread, or delaying life-saving surgery. Three imaging tools dominate this space: PET-CT, MRI, and the newer PET-MRI. Each has strengths, weaknesses, and situations where one clearly outperforms the others. There’s no single best option. The right choice depends on the cancer type, where it’s located, and what question the doctor is trying to answer.
PET-CT: The workhorse of cancer staging
PET-CT became the standard in the early 2000s after its first commercial system launched in 2001. It combines two scans into one: a PET scan that shows where cancer cells are metabolically active, and a CT scan that maps the body’s anatomy. The tracer used is usually 18F-FDG, a sugar-like molecule that cancer cells gobble up faster than normal tissue. This makes tumors light up on the scan.
It’s fast-most scans take 15 to 20 minutes per patient. It’s widely available, even in community hospitals. And it’s excellent at spotting cancer that’s spread beyond the original site, especially in lymph nodes, lungs, and bones. For non-small cell lung cancer, Hodgkin’s lymphoma, and melanoma, PET-CT is often the first and sometimes the only scan needed for staging.
But it has limits. It struggles with cancers that don’t use a lot of sugar, like some prostate or kidney cancers. It also can’t tell the difference between a tumor and inflammation, which can lead to false positives. And while it gives good anatomical detail, it’s not as sharp as MRI when it comes to soft tissues like the liver, brain, or pelvic organs. The radiation dose? Between 10 and 25 mSv-roughly equivalent to 3 to 5 years of natural background radiation.
MRI: The detail king without radiation
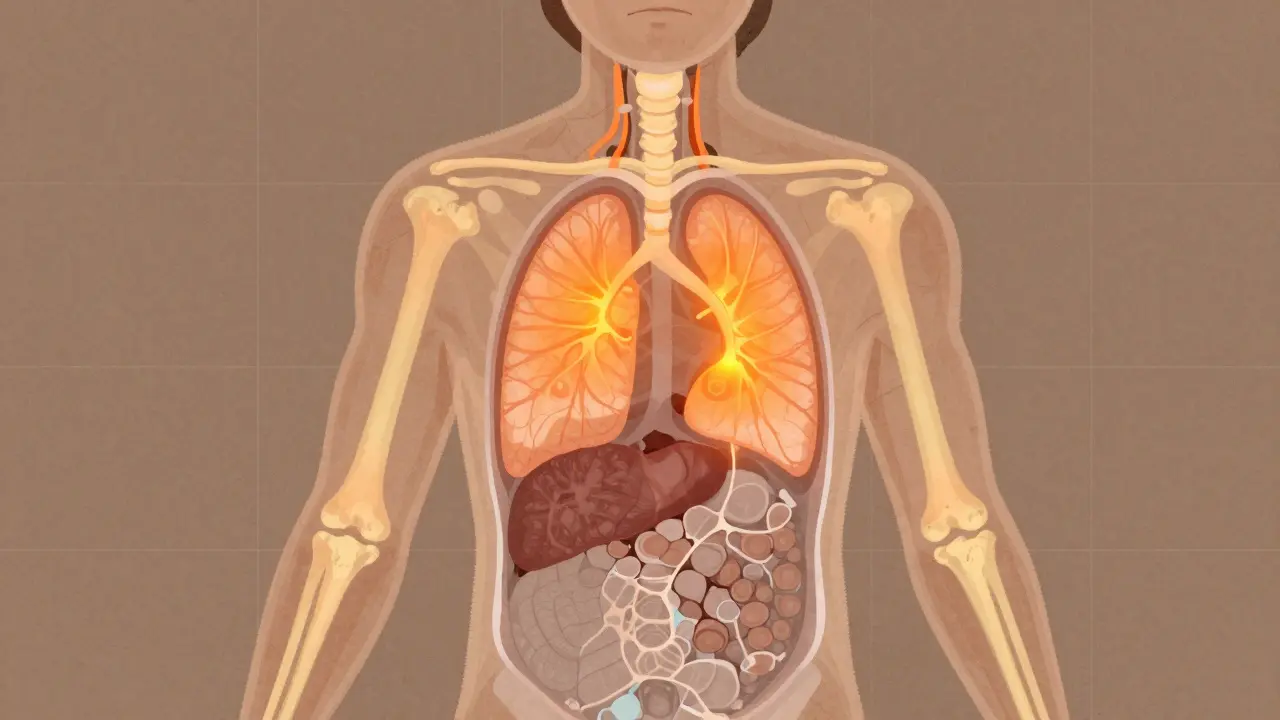
MRI doesn’t use radiation. Instead, it uses powerful magnets and radio waves to create incredibly detailed pictures of soft tissues. Since the 1980s, it’s been the go-to for brain tumors, spinal cord cancers, liver lesions, and pelvic cancers like prostate and cervical cancer.
At 3 Tesla strength-the standard for oncology-MRI can show structures down to 0.5 mm. Functional techniques like diffusion-weighted imaging (DWI) help detect tumors based on how water moves inside cells, which changes when cancer is present. For prostate cancer, multiparametric MRI is now the frontline tool before biopsy. In breast cancer, it’s used for high-risk screening and checking how well chemotherapy is working.
But MRI has downsides. It’s slow. A full-body or complex pelvic MRI can take 30 to 60 minutes. Patients have to lie perfectly still. Motion-like breathing or even a slight twitch-can blur the images. It’s also noisy, claustrophobic for some, and unsafe for people with certain metal implants like pacemakers or old aneurysm clips. And unlike PET-CT, MRI doesn’t show metabolic activity. A mass could be cancer, scar tissue, or a benign growth. That’s why MRI alone isn’t enough for full staging in many cases.

PET-MRI: The hybrid that’s changing the game
PET-MRI, first approved in 2011, merges the metabolic power of PET with the soft-tissue clarity of MRI in a single machine. It’s not just a combo-it’s a synergy. You get cancer’s metabolic activity mapped onto ultra-detailed anatomy, all in one session.
This matters most in tricky cases. For brain tumors, PET-MRI can tell whether a growing area after treatment is new cancer or just radiation damage-a distinction MRI alone gets wrong up to 30% of the time. PET-MRI gets it right 85-90% of the time. In liver cancer, it spots small metastases that PET-CT misses. In pediatric cancers, it cuts radiation exposure by about half compared to PET-CT, which is a big deal for kids who may need scans over many years.
But it’s not perfect. The biggest technical headache? Attenuation correction. Because MRI doesn’t measure density like CT does, the PET part of the scan can get distorted without special software. Siemens and other manufacturers have improved this with Dixon-based algorithms, but it still causes artifacts in 63% of centers, according to a 2022 study. The scan takes longer-45 to 60 minutes-and requires highly trained staff. Fewer than 1 in 5 U.S. hospitals have it.
Which scan for which cancer?
Choosing between these tools isn’t about which is “better.” It’s about which is right for the job.
- For lung, lymphoma, or melanoma: PET-CT is still the gold standard. It’s fast, proven, and shows spread clearly.
- For prostate cancer: PSMA PET-CT is becoming standard for advanced cases, but multiparametric MRI is used first for initial diagnosis. Some centers now use PSMA PET-MRI for precise staging.
- For breast cancer: MRI is best for evaluating tumor size and response to chemo, especially in dense breasts. PET-CT adds value if there’s suspicion of distant spread.
- For pancreatic cancer: A 2023 study found PET-MRI changed treatment plans for nearly half of patients compared to standard imaging.
- For brain tumors: PET-MRI is unmatched for distinguishing recurrence from treatment effects.
- For children or young adults: PET-MRI is preferred when possible to reduce lifetime radiation exposure.
Cost, access, and real-world challenges
PET-CT systems cost $1.8 to $2.5 million. PET-MRI? $3 to $4.2 million. That’s a huge difference for hospitals. Add in the cost of shielding-$150,000 for an MRI room versus $50,000 for PET-CT-and the gap widens.
Reimbursement is another hurdle. In the U.S., PET-MRI often costs $2,500 to $3,500 per scan, compared to $1,600 to $2,300 for PET-CT. Insurance doesn’t always cover it unless there’s a clear clinical need. Many centers use PET-MRI only for select cases: recurrent cancer, pediatric tumors, or when PET-CT results are unclear.
Training is a barrier too. Radiologists need 6-12 months to master PET-CT interpretation. For PET-MRI, add another 3-6 months. Technologists need 40+ extra hours of training. In a 2022 survey, 45% of cancer centers said workflow integration was their biggest challenge.
The future: AI, new tracers, and smarter choices
The next wave isn’t just better machines-it’s smarter interpretation. At the 2023 RSNA meeting, over two dozen studies showed how AI can analyze PET-MRI data to predict how a tumor will respond to treatment before it even shrinks. This is called radiomics-turning images into data.
New tracers are also expanding what we can see. PSMA for prostate cancer, Ga-68 DOTATATE for neuroendocrine tumors, and F-18 DOPA for brain tumors are giving us more precise targets than the old FDG tracer. Some centers are now combining these with multiparametric MRI in a single PET-MRI scan.
The 2024 ASCO guidelines now recommend imaging choices based on tumor biology, not just location. That’s a big shift. It means a patient with triple-negative breast cancer might get a different scan than someone with hormone-positive disease-even if both have the same stage.
By 2035, experts predict PET-MRI will make up 25-30% of oncologic imaging in academic centers. But PET-CT won’t disappear. It’s too practical, too fast, too widespread. The future isn’t one tool replacing another. It’s using the right tool, at the right time, for the right patient.
What patients should know
If you’re facing cancer staging, ask your doctor: Why this scan? What are we looking for? What happens if the result is unclear? Don’t assume more expensive means better. A PET-MRI isn’t always needed. A simple MRI or PET-CT might be enough.
If you’re a child, young adult, or need multiple scans over time, ask about radiation exposure. PET-MRI reduces that risk. If you have metal implants, MRI may not be an option-ask about alternatives.
And if your scan results are confusing? Get a second opinion from a specialist in oncologic imaging. These tools are powerful, but they’re not infallible. Expert interpretation makes all the difference.
Is PET-CT or MRI better for cancer staging?
Neither is universally better-it depends on the cancer type. PET-CT excels at finding spread to lymph nodes, lungs, and bones, especially in lung cancer and lymphoma. MRI is superior for soft tissue detail, making it ideal for brain, liver, prostate, and pelvic cancers. For many cancers, the two are used together or in sequence to get a full picture.
Does PET-MRI replace PET-CT?
Not yet. PET-MRI offers better detail in specific cancers like brain tumors, liver metastases, and pediatric cases, and reduces radiation. But it’s slower, more expensive, and less available. PET-CT remains the workhorse for most patients because it’s faster, cheaper, and widely accessible. PET-MRI is reserved for complex cases where its advantages clearly impact treatment.
How accurate is MRI for detecting cancer spread?
MRI is highly accurate for local spread-like whether a prostate tumor has invaded nearby tissue or if a liver lesion is cancerous. But it’s less reliable for spotting tiny metastases in distant organs like bones or lungs. That’s where PET-CT adds value. For full staging, MRI often needs to be paired with a metabolic scan like PET.
Why is PET-MRI so expensive?
PET-MRI machines cost over $3 million, nearly double the price of PET-CT. They require specialized rooms with magnetic shielding ($150,000+), advanced software for image fusion, and highly trained staff. Maintenance and calibration are complex. The higher cost is justified only in cases where diagnostic accuracy significantly changes treatment-like distinguishing tumor recurrence from radiation damage in the brain.
Are there risks from radiation in PET-CT scans?
Yes. A typical PET-CT scan delivers 10-25 mSv of radiation-equivalent to several years of natural background exposure. While this level is considered safe for adults needing cancer care, repeated scans over time increase cumulative risk. For children, young adults, and patients needing long-term monitoring, PET-MRI is preferred because it cuts radiation by about half. The goal is always to use the lowest dose necessary to get the answer.
What’s next for cancer imaging?
The next five years will see AI play a bigger role-predicting tumor behavior from imaging patterns before any treatment starts. New radiotracers will target more cancer types with greater precision. And as costs come down, PET-MRI will move out of academic centers and into larger hospitals.
But the core principle won’t change: imaging isn’t about taking pictures. It’s about answering clinical questions. The best scan is the one that gives the right answer, at the right time, with the least harm. That’s what guides real-world decisions-not marketing, not hype, but evidence, experience, and patient need.

Gregory Parschauer
January 15, 2026 AT 11:01Let me be crystal clear: if your hospital is still using PET-CT as a first-line tool for prostate or brain cancer, you're practicing 2010 medicine. PET-MRI isn't some luxury toy-it's the only way to reliably distinguish radiation necrosis from recurrence. I've seen patients get radical resections because their PET-CT was misread as stable disease. That's malpractice waiting to happen. And don't even get me started on how radiologists still treat MRI like a pretty picture instead of a functional biomarker. We're not in the dark ages anymore.
Damario Brown
January 16, 2026 AT 19:09lol so pet ct is dead? bro i work in a rural hospital and we got one pet ct that’s booked 3 weeks out. pet mri? we dont even have a working mri that dont make people panic. also the doc told me 18f-fdg is sugar but its not sugar its a tracer. why u always gotta be so extra?
sam abas
January 18, 2026 AT 02:16Okay, but if you look at the 2023 meta-analysis from the Journal of Nuclear Medicine, the sensitivity of PET-CT for nodal staging in NSCLC is 87% versus 91% for PET-MRI-but the specificity drops from 92% to 84% because of motion artifacts and attenuation errors. And that’s assuming the center has a certified PET-MRI physicist, which less than 12% of community hospitals do. So while the tech is sexy, the real-world impact? Marginal. And let’s not pretend insurance is gonna pay $3,500 for a scan that doesn’t change management in 60% of cases. The ‘gold standard’ label is a marketing term, not a clinical one.
Priyanka Kumari
January 18, 2026 AT 19:19This is such an important breakdown. I’ve worked with patients who were terrified their MRI meant ‘cancer everywhere’-only to find out it was just inflammation. Or those who refused PET-CT because they thought radiation would ‘burn’ their body. The clarity here helps demystify what can feel like a scary, opaque process. I’ve shared this with my oncology support group-thank you for explaining the why behind the scans, not just the what. Knowledge truly is power when you’re facing a diagnosis.
Alan Lin
January 20, 2026 AT 09:22It is imperative that we recognize the profound ethical implications of imaging modality selection. The disparity in access between academic medical centers and rural facilities constitutes a systemic inequity in oncologic care. Furthermore, the financial burden imposed upon patients by out-of-pocket expenses for PET-MRI-despite its superior diagnostic accuracy-represents a violation of the principle of justice in medical ethics. We must advocate for policy reform that ensures equitable access to advanced imaging, irrespective of socioeconomic status or geographic location. The standard of care must not be dictated by hospital budgets.
Rosalee Vanness
January 21, 2026 AT 08:15I remember sitting in that radiology waiting room with my mom, clutching her hand, listening to the MRI machine sound like a drum circle gone rogue. She was so scared they’d find something worse. Then the doc showed us the scan-clear as glass, every little nodule mapped out. No radiation, no guesswork. I cried. Not because it was bad news, but because for once, we had clarity. That’s what MRI gave us. And yeah, it took forever. But sometimes, slow is sacred. I wish more people understood that the quiet hum of a magnet can be more comforting than the buzz of a radioactive tracer.
John Tran
January 22, 2026 AT 18:08Think about it: we’re mapping the soul of cancer through electromagnetic fields and sugar analogs. PET-MRI doesn’t just show tumors-it reveals the metabolic whisper of cellular rebellion. We’re not technicians, we’re alchemists turning photons into prophecy. And yet, the system treats this like a vending machine: insert insurance, receive scan. Where’s the reverence? Where’s the poetry of seeing a tumor glow like a dying star in the dark? We’ve quantified everything and forgotten why we started-because life is sacred, and we owe it to the patient to see it fully, not just clearly.
Trevor Whipple
January 23, 2026 AT 01:47pet-mri my ass. i saw a guy with prostate cancer get a pet-mri and they still missed the bone mets. then he got a bone scan and boom. there it was. so all that fancy tech and you still need the dumb ol’ bone scan? yeah right. also who the hell pays 3 mill for a machine? your hospital is broke and you’re spending it on sci-fi gadgets. stick with pet-ct and save the cash for actual meds.
Lethabo Phalafala
January 24, 2026 AT 17:23My cousin was diagnosed with neuroendocrine cancer at 28. They did a Ga-68 DOTATATE PET-MRI and found five tiny metastases in her liver-ones the PET-CT missed. That one scan changed everything. She went from palliative chemo to targeted therapy and has been in remission for two years now. I’m not saying PET-MRI is magic-but when it works, it’s like the universe leans in and whispers, ‘We’ve got you.’ Don’t dismiss it because it’s expensive. Some things are worth the cost.
Lance Nickie
January 25, 2026 AT 00:19pet-ct is fine. stop overcomplicating it.
Milla Masliy
January 25, 2026 AT 11:22In my village in South Africa, we don’t have PET scanners at all. But we have community health workers who use clinical exams, ultrasound, and basic blood tests to catch cancer early. I’ve seen people survive because someone noticed a lump and walked them to the clinic. This post is brilliant-but it’s written for hospitals with $4 million machines. Let’s not forget the millions who don’t have access to any of this. Maybe the real innovation isn’t the machine-it’s making sure someone, anywhere, gets seen.