Introduction to Meloxicam and Asthma
As a blogger, I often come across the topic of medications and their potential side effects. One such medication that has caught my attention is Meloxicam, a nonsteroidal anti-inflammatory drug (NSAID) commonly prescribed for pain relief and inflammation. While this medication can be beneficial for many patients, there are potential risks associated with its use, particularly for individuals with asthma. In this article, I will be discussing these risks and providing information on what to consider if you or a loved one have asthma and are prescribed Meloxicam.
Understanding Meloxicam
Before diving into the potential risks of Meloxicam for asthma patients, it is essential to understand what this medication is and how it works. Meloxicam is an NSAID that helps to reduce inflammation and pain by blocking the production of prostaglandins, chemicals responsible for causing inflammation, pain, and fever in the body. It is commonly prescribed for conditions such as osteoarthritis, rheumatoid arthritis, and other inflammatory conditions.
Asthma and NSAIDs
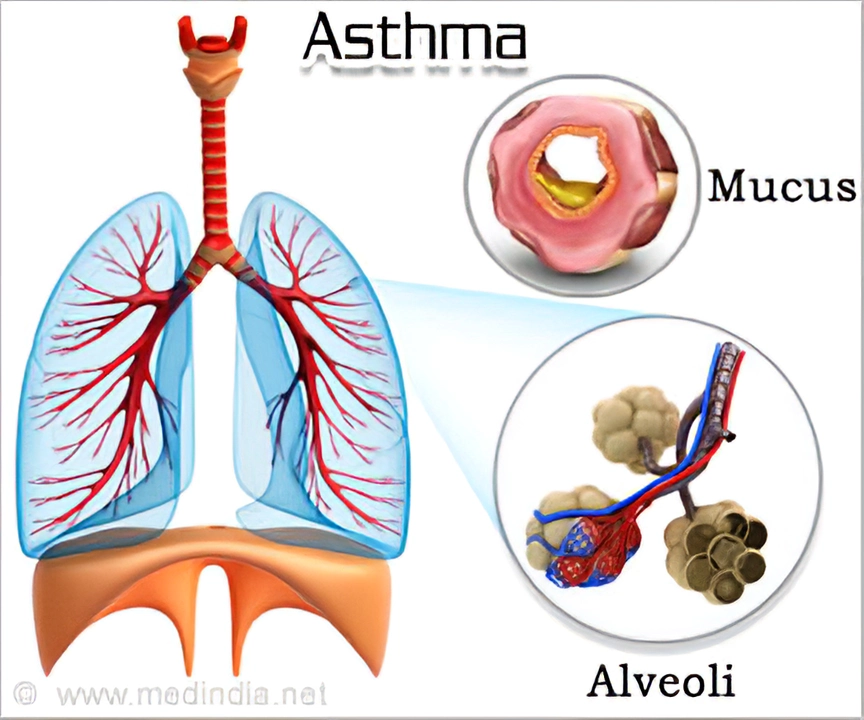
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to difficulty breathing, chest tightness, coughing, and wheezing. For some individuals with asthma, certain medications, including NSAIDs, can exacerbate asthma symptoms or even cause an asthma attack. This is known as NSAID-exacerbated respiratory disease (NERD) and affects approximately 10% of adults with asthma.
How Meloxicam May Affect Asthma
While Meloxicam may not directly cause asthma, it can potentially worsen asthma symptoms in some individuals. This is because NSAIDs like Meloxicam can inhibit the production of prostaglandins, which can lead to an imbalance in the production of other chemicals called leukotrienes. Leukotrienes are responsible for causing inflammation and narrowing of the airways in asthma. Therefore, by inhibiting prostaglandin production, Meloxicam may indirectly increase the production of leukotrienes, exacerbating asthma symptoms.
Recognizing the Signs of an Asthma Attack
If you or a loved one have asthma and are taking Meloxicam, it is crucial to be aware of the signs of an asthma attack. These may include sudden shortness of breath, worsening of wheezing or coughing, chest tightness or pain, and difficulty speaking. If you notice any of these signs while taking Meloxicam, seek immediate medical attention.
Alternatives to Meloxicam for Asthma Patients
If you have asthma and are concerned about the potential risks of taking Meloxicam, it is essential to discuss these concerns with your healthcare provider. They may recommend alternative medications to help manage your pain and inflammation. Some alternatives may include acetaminophen, which is not an NSAID and does not carry the same risks for asthma patients, or selective COX-2 inhibitors, which may have fewer respiratory side effects than traditional NSAIDs.
Managing Asthma While Taking Meloxicam
If your healthcare provider determines that Meloxicam is the best option for your needs, it is essential to take steps to manage your asthma effectively while taking this medication. This may include using your asthma medications as prescribed, monitoring your asthma symptoms closely, and having an up-to-date asthma action plan in place. Additionally, keep open communication with your healthcare provider about any changes in your asthma symptoms or concerns about your medications.
Conclusion: Weighing the Risks and Benefits
Ultimately, the decision to use Meloxicam or any other medication should be based on a careful evaluation of the potential risks and benefits. For some individuals with asthma, the benefits of Meloxicam for managing pain and inflammation may outweigh the potential risks. However, for others, alternative medications may be a safer option. It is essential to have open and honest conversations with your healthcare provider about your asthma and any concerns you may have about your medications, so you can make the best decision for your health and well-being.

Shaun Brown
May 6, 2023 AT 22:23First off, let me just say that the whole NSAID‑asthma link is not some new conspiracy theory concocted by the pharmaceutical industry to keep us scared, it's a well‑documented physiological phenomenon that’s been studied for decades. When you take a drug like meloxicam, you’re essentially throwing a wrench into the prostaglandin pathway, which, while helpful for reducing pain, also means you’re shifting the balance toward leukotriene production. For an asthmatic whose airways are already hypersensitive, that shift can be the difference between a mild cough and a full‑blown bronchospasm. The literature points out that roughly ten percent of adult asthmatics have NSAID‑exacerbated respiratory disease, and that’s not a trivial number when you consider the millions of people on these meds. Moreover, the risk isn’t uniform; patients with severe, poorly controlled asthma are far more likely to experience an adverse reaction than those with mild, intermittent symptoms. What’s more, the onset can be insidious – you might not notice the subtle increase in wheezing until it escalates into a genuine attack, which is why vigilant monitoring is crucial. The standard recommendation to switch to acetaminophen or a selective COX‑2 inhibitor isn’t just a convenience, it’s a safety measure backed by pharmacologic logic. If you’re already on a regimen that includes inhaled corticosteroids, you still need to be wary because the anti‑inflammatory effects of your asthma meds can be overridden by the sudden surge in leukotrienes caused by the NSAID. And let’s not forget drug interactions – combining meloxicam with certain beta‑agonists or leukotriene modifiers can create unexpected side effects that further compromise respiratory function. In practice, a good clinician will take a detailed medication history, ask about known NSAID sensitivities, and perhaps even perform an oral challenge under supervision if the history is ambiguous. Bottom line: meloxicam can be a useful analgesic, but for anyone with a history of asthma, especially if it’s been diagnosed as NERD, the risk‑benefit calculus should be reassessed on a case‑by‑case basis. Don’t just assume that because you’ve tolerated ibuprofen in the past, meloxicam will be a safe switch – the pharmacodynamics are different enough to warrant caution. Finally, if you or a loved one does experience sudden shortness of breath, chest tightness, or an inability to speak in full sentences while on meloxican, treat it as a medical emergency and seek help immediately.
Damon Dewey
May 13, 2023 AT 15:32That whole NSAID‑asthma thing is overblown, but if you’re already wheezing, better ditch the meloxicam.
Dan Barreto da Silva
May 20, 2023 AT 08:41Yo, listen up! I’ve seen my cousin’s asthma flare up after he popped a painkiller, and he swore he felt like he was drowning. The drama of trying to catch his breath while the world keeps spinning is real, and nobody wants that on a day they’re already dealing with a broken ankle. So yeah, meloxicam might be tasty for the joints, but it can be a literal fire‑starter for the lungs. If you love drama, just keep the drama inside your chest and avoid the trigger. Trust me, you don’t need that extra thrill when you can just binge‑watch a series instead.
Ariel Munoz
May 27, 2023 AT 01:49Look, I’m not here to sugarcoat anything – the American healthcare system loves dumping meds on us whether we need them or not. You think meloxicam is just a harmless pill? Wrong. It’s a tool of the pharmaceutical oligarchy to keep you dependent while potentially wrecking your respiratory system. If you’ve got asthma, you should be demanding alternatives, not quietly swallowing whatever the doctor prescribes. It’s a matter of national pride to stand up against these invasive drugs that threaten our health. Don’t let the “doctor knows best” mantra silence your own body’s warnings.
Ryan Hlavaty
June 2, 2023 AT 18:58We have a moral responsibility to protect vulnerable individuals from unnecessary risks. If a medication like meloxicam poses a documented danger to asthmatics, it should be prescribed with utmost caution, if at all. It’s not just a medical decision; it’s an ethical one. We must prioritize safety over convenience and ensure patients are fully informed.
Chris Faber
June 9, 2023 AT 12:06Hey, I get where you’re coming from but maybe there’s a middle ground. Talk to your doc about a trial with a lower dose or a different drug like acetaminophen. Keeping the conversation open can help you find something that eases pain without risking a flare‑up. No need to go full panic mode.
aura green
June 16, 2023 AT 05:15Alright, let’s get real for a sec – the world isn’t going to end because you take meloxicam, but your lungs might not be thrilled about the side‑effects. It’s like that old saying, “Don’t bite the hand that feeds you” except here the hand is a drug that could hand you a cough. I mean, if you love drama (and who doesn’t?), you might think a little wheeze adds spice, but trust me, it’s not the kind of excitement you want. So, maybe consider a different pain reliever, especially if your asthma has a mind of its own. And hey, if you’re already on meloxicam and feeling fine, keep an eye out – a sudden gasp for air isn’t a great party trick. Stay safe, keep your inhaler handy, and don’t let the medication be the villain in your health story. 😊
Edward Morrow
June 22, 2023 AT 22:23Just ditch it, mate.