Liver Drug Dose Adjuster
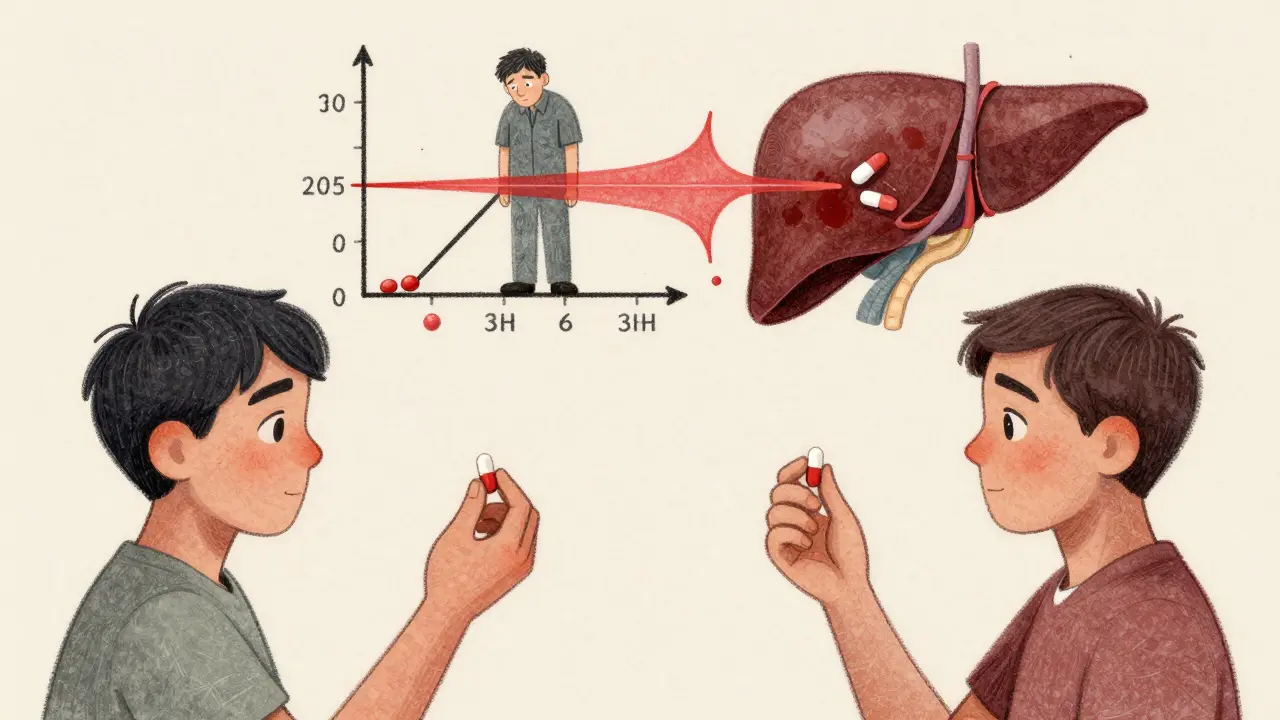
This tool calculates how liver disease affects medication clearance using the MELD score. Enter your MELD score and select a drug to see the recommended dose adjustment.
Recommended Dose Adjustment
When your liver is damaged, it doesn’t just affect how you feel-it changes how every pill you take works in your body. Many people don’t realize that common medications like painkillers, sedatives, and antibiotics can become dangerous if you have liver disease. The problem isn’t always obvious. You might take the same dose you’ve always taken, but your body processes it differently. That’s because liver disease cuts drug clearance by 30% to 50%, and in severe cases, even more. This isn’t theoretical-it’s happening right now in millions of people, and it’s leading to overdoses, hospitalizations, and treatment failures.
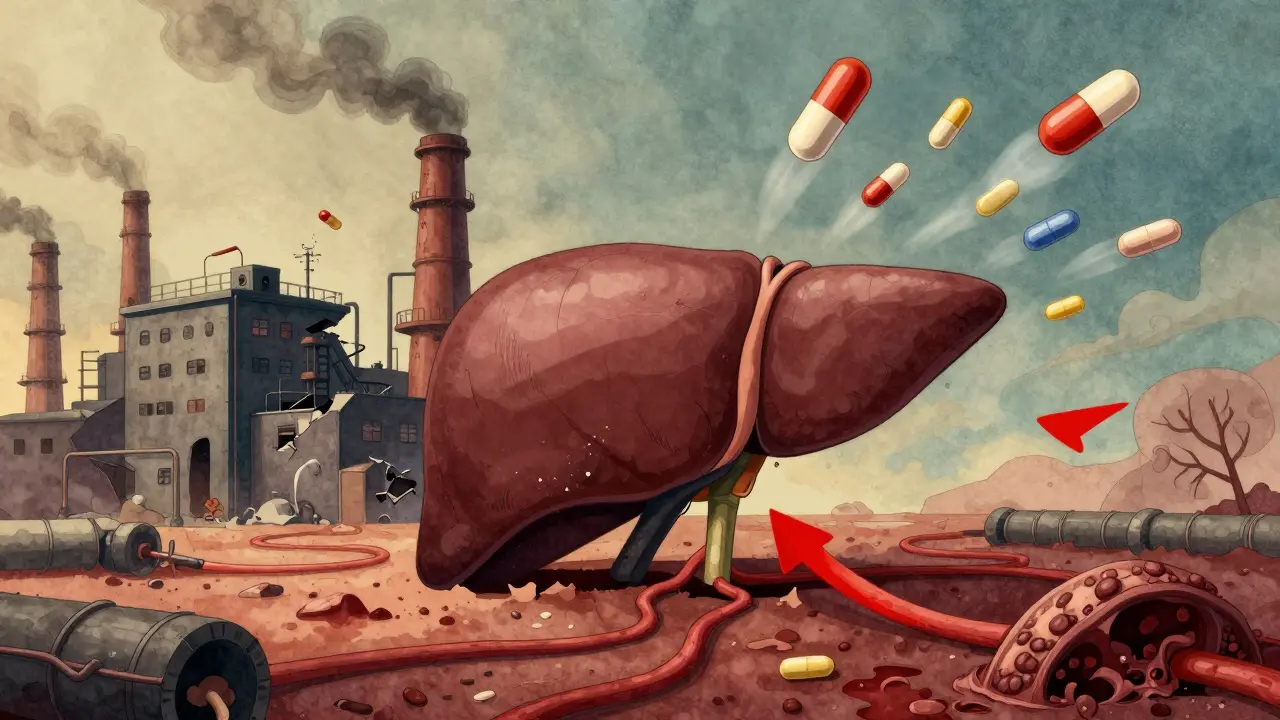
Why the Liver Matters for Every Drug You Take
Your liver doesn’t just filter toxins. It’s the main factory that breaks down most medications. About 70% of the drugs people take daily-like antidepressants, blood pressure pills, and opioids-are processed by liver enzymes. These enzymes, especially the CYP450 family (like CYP3A4 and CYP2E1), chemically change drugs so they can be eliminated from your body. But when liver disease sets in, these enzymes slow down. In advanced cirrhosis, CYP3A4 activity drops by 30% to 50%. CYP2E1 can fall by as much as 60%. That means drugs stick around longer, building up in your bloodstream.
It’s not just enzymes. The liver’s physical structure changes too. Scar tissue blocks blood flow. Blood vessels reroute, letting drugs bypass the liver entirely through portosystemic shunts. Up to 40% of blood can flow around the liver instead of through it. That means oral drugs like fentanyl or morphine get absorbed faster and stronger than they should. Your body doesn’t get a chance to break them down before they reach your brain.
High-Extraction vs. Low-Extraction Drugs: What’s the Difference?
Not all drugs are affected the same way. The key is whether a drug is high-extraction or low-extraction. High-extraction drugs (like fentanyl, morphine, and propranolol) rely heavily on liver blood flow. When blood flow drops in cirrhosis, these drugs aren’t cleared as quickly. But here’s the catch: because they’re so efficiently removed in healthy people, even small drops in flow cause big changes in their levels.
Low-extraction drugs (like diazepam, lorazepam, and methadone) are broken down by enzymes, not blood flow. These make up the majority of prescriptions. In liver disease, these are the real hidden danger. Their clearance depends on enzyme activity-which declines sharply. A standard dose of diazepam might stay in your system for days instead of hours. That’s why sedatives are so risky in people with cirrhosis. Even small amounts can cause confusion, drowsiness, or coma.
How Liver Damage Changes Drug Behavior
It’s not just about slower breakdown. Liver disease alters every step of a drug’s journey:
- Protein binding: Many drugs attach to proteins in the blood. In liver disease, albumin drops, so more free drug circulates-increasing its effect.
- Biliary excretion: Some drugs leave the body through bile. Scarred livers can’t push bile out properly, causing drugs to build up.
- Enterohepatic circulation: Some drugs are reabsorbed from the gut after being excreted in bile. Liver disease disrupts this cycle unpredictably.
- Renal clearance: Even though the kidneys handle excretion, liver disease can damage them too, especially in advanced cases.
One study found that patients with cirrhosis had 40-60% higher peak levels of ceftriaxone-a common antibiotic-after a standard dose. That’s not a small increase. It’s enough to cause toxicity.
Real-World Examples: Which Drugs Are Most Risky?
Some drugs are known killers in liver disease. Here’s what happens:
- Warfarin: Clearance drops by 30-50%. A standard dose can push INR levels into dangerous territory. Dose reductions of 25-40% are often needed.
- Diazepam: Has active metabolites that last for days. In cirrhosis, dose reductions of 50-70% are recommended.
- Lorazepam: No active metabolites. Safer. Still needs a 25-40% reduction.
- Opioids: Even small doses can trigger hepatic encephalopathy. Fentanyl and oxycodone require at least 50% dose cuts in moderate cirrhosis.
- Sugammadex: Mostly cleared by kidneys. No dose change needed-but recovery time from muscle paralysis is 40% longer.
And here’s the twist: not every bad reaction comes from higher drug levels. Some patients have a lower tolerance. Their brains are more sensitive. A dose that’s safe for a healthy person can cause confusion or coma in someone with cirrhosis-even if blood levels are normal.
How Doctors Measure Liver Damage (And Why It Matters)
You can’t rely on a single blood test. AST and ALT levels? Often normal in cirrhosis. Bilirubin? Only rises late. The real tools are the Child-Pugh and MELD scores.
Child-Pugh scores use five things: bilirubin, albumin, INR, ascites, and encephalopathy. Class A = mild, B = moderate, C = severe. In Child-Pugh B, drug clearance drops 25-45%. In Class C, it drops 50-75%. That’s not a suggestion-it’s a red flag.
MELD score? It’s even more precise. For every 5-point increase above 10, drug clearance drops by about 15%. A MELD of 20 means you’re clearing drugs at half the rate of a healthy person.
Doctors now use these scores to guide dosing-not just liver enzymes.
When You Don’t Need to Change the Dose
Not every drug needs adjustment. The FDA says two cases are safe:
- Drugs cleared almost entirely by the kidneys (like sugammadex, vancomycin, or most antibiotics).
- Drugs with minimal liver metabolism (less than 20%) and a wide safety margin (like acetaminophen at low doses, or some antihistamines).
But even then, caution is needed. A drug might be safe in theory-but if you’re also on other meds, or have kidney problems, or are dehydrated, the risk spikes.
What’s New in Dosing? The Rise of Model-Based Precision
Old-school dosing-"reduce by half"-is outdated. New tools are changing the game.
Physiologically based pharmacokinetic (PBPK) modeling uses computer simulations to predict how a drug behaves in a liver-damaged body. It factors in blood flow, enzyme levels, shunting, and even body weight. These models are now 85-90% accurate. The FDA is pushing for their use in drug labels.
Soon, instead of saying "reduce dose in liver disease," labels will say: "For MELD 15-20, use 60% of standard dose. For MELD >25, avoid."
And it’s not just theory. A 2023 study showed that using these models to personalize doses cut adverse drug events by 34% in cirrhotic patients.

The Bigger Picture: Why This Is Getting Worse
More people have liver disease than ever. Over 22 million Americans have chronic liver disease. One in three has fatty liver-even if they’re not overweight. And that early fatty liver? It already reduces CYP3A4 activity by 15-25%. That means even people with "mild" liver damage need to rethink their meds.
Drug companies are responding. In 2023, 18 new drugs came with liver-specific dosing instructions. That’s 25% more than the year before. By 2026, the market for therapeutic drug monitoring in liver disease will hit $1.24 billion. Pharmacists are now running specialized clinics to adjust doses.
But here’s the problem: most patients don’t know. Most primary care doctors don’t check MELD scores. Most pharmacists still rely on outdated rules.
What You Can Do
If you or someone you care for has liver disease:
- Ask your doctor: "What’s my Child-Pugh or MELD score?"
- Ask your pharmacist: "Do any of my meds need a dose change because of my liver?"
- Never assume a dose is safe just because it’s "standard."
- Watch for signs of toxicity: confusion, extreme drowsiness, unsteady walking, nausea, or vomiting.
- If you’re on warfarin, opioids, or benzodiazepines-get your levels checked regularly.
There’s no magic fix. But awareness saves lives. A simple question-"Is my dose right for my liver?"-can prevent an overdose, a coma, or a hospital stay.
Final Thought: It’s Not About the Drug. It’s About the Body.
Medications aren’t one-size-fits-all. Your liver isn’t just a filter. It’s a complex, dynamic system. When it’s damaged, your body becomes a different place for drugs to live in. What worked yesterday might kill you tomorrow. That’s why we need to stop thinking about dosing as a static number-and start treating it like a living, changing system. Because in liver disease, the only safe dose is the one that’s personalized to you.

Paul Ong
January 1, 2026 AT 15:01Man i just took a vicodin last week for my back and never even thought about my liver
Richard Thomas
January 3, 2026 AT 14:02It’s fascinating how we treat medications like abstract quantities rather than dynamic entities interacting with a biological system that’s constantly changing. The liver isn’t a broken pipe you fix with a wrench-it’s a living factory with shifting output, rerouted pipelines, and failing machinery. When you reduce a dose by half because someone has cirrhosis, you’re not just adjusting for pharmacokinetics-you’re acknowledging that the person’s entire internal chemistry has been rewritten. And yet, we still prescribe like everyone’s physiology is a standardized model from 1998. The real tragedy isn’t the overdose-it’s that we keep pretending we can treat complex biology with bullet points on a checklist.
Todd Nickel
January 4, 2026 AT 09:35There’s a critical gap between what the literature says and what’s actually practiced. PBPK modeling is precise, validated, and increasingly accessible-but most primary care providers still rely on the old "reduce by 50%" heuristic because it’s easier than looking up MELD scores or consulting a clinical pharmacist. The disconnect isn’t ignorance; it’s systemic inertia. Electronic health records don’t auto-flag high-risk meds based on liver function. Prescribing interfaces don’t prompt for dose adjustments. Even when the science is clear, the infrastructure hasn’t caught up. Until dosing algorithms are baked into the workflow, not just the textbooks, this will keep happening.
Ann Romine
January 5, 2026 AT 07:37I’ve seen this with my mother. She had fatty liver from years of drinking, not obesity. She was on a low dose of diazepam for anxiety and ended up in the ER after a simple dose increase. No one asked about her liver function. The ER doctor just said "she’s sensitive to meds." But it wasn’t sensitivity-it was metabolism. We didn’t know to ask for Child-Pugh or MELD. Now I carry a printed list of safe meds for her. It’s not paranoia-it’s survival. I wish more families had this knowledge before it’s too late.
gerard najera
January 6, 2026 AT 17:29Drugs aren’t magic. Your liver decides if they work or kill you.
Austin Mac-Anabraba
January 6, 2026 AT 17:39Of course the pharmaceutical industry is pushing "personalized dosing." They’ve been doing this since the 70s-create a problem, then sell the solution. They don’t care if you live or die, only if you keep buying their pills. Now they’re slapping "MELD-adjusted" labels on everything so they can charge more. Real medicine used to be about simplicity: less is more. Now it’s about complexity so they can patent new versions of old drugs. Wake up. This isn’t progress-it’s profit engineering.
Phoebe McKenzie
January 8, 2026 AT 12:16YOU’RE ALL IGNORANT. NO ONE TELLS YOU THIS BECAUSE THE GOVERNMENT AND BIG PHARMA WANT YOU DEAD. THEY LET PEOPLE GET LIVER DISEASE ON PURPOSE SO THEY CAN SELL MORE DRUGS. DID YOU KNOW THAT ACETAMINOPHEN WAS DESIGNED TO BE SAFE-UNTIL THEY FOUND OUT IT KILLS PEOPLE WITH LIVER DAMAGE? NOW THEY TELL YOU TO "BE CAREFUL" SO THEY DON’T GET SUED. THEY’RE KILLING YOU WITH YOUR OWN MEDS AND CALLING IT "MEDICINE." STOP TRUSTING DOCTORS. ASK FOR YOUR LIVER SCORE OR YOU’LL BE NEXT.
Andy Heinlein
January 8, 2026 AT 12:41just found out my cousin’s on 3 meds that probably shouldn’t be near his liver… thanks for this post man 😅 i’m gonna make him call his doc this week. no joke, i didn’t even know liver disease could mess with pills like this. kinda scary but also kinda empowering to know what to ask for now
Stephen Gikuma
January 9, 2026 AT 15:19They’re pushing this "MELD score" nonsense because they want to control your body. Who decides what your liver can handle? The same people who told you vaccines were safe. This is all part of the medical-industrial complex. They don’t want you healthy-they want you dependent. If you’re on meds, you’re a customer. If you’re off meds, you’re a threat. Your liver isn’t broken-it’s being poisoned by the system. Don’t let them label you. Fight back.
Bobby Collins
January 11, 2026 AT 07:40okay but like… what if your liver is messed up from weed? like, is that even counted? because i heard it messes with cyp enzymes too and no one ever talks about that
Layla Anna
January 11, 2026 AT 17:40my grandma had cirrhosis and took lorazepam for years… she never had a problem until they added a new antibiotic. then she got so confused she didn’t recognize me for three days 😢 i wish someone had told us earlier. thank you for writing this. i’m sharing it with my whole family now 🤍