Why Checking Your Medication Label Matters
Every time you pick up a prescription, the label on the bottle is your first and most reliable line of defense against dangerous mistakes. It’s not just a piece of paper with your name and dosage-it’s a safety checklist. The prescriber’s name, the pharmacy’s contact info, the prescription number: all of these details are there for a reason. If something looks off, it might be saving your life.
According to the FDA, over 1.3 million people in the U.S. are injured each year because of medication errors. About 12% of those errors happen because the prescriber or pharmacy information on the label doesn’t match what’s supposed to be there. That’s not a small risk. It’s the kind of mistake that can lead to taking the wrong drug, a dangerous interaction, or even a life-threatening reaction.
And here’s the thing: you don’t need to be a doctor to catch these errors. You just need to know what to look for-and how to double-check it.
What Information Must Be on the Label
By law, every prescription label in the U.S. must include specific details. If any of these are missing, the pharmacy is out of compliance. Here’s what you should see:
- Prescriber’s full name-This is the doctor, nurse practitioner, or other licensed provider who wrote the prescription. It should match exactly who you saw.
- National Provider Identifier (NPI) number-A unique 10-digit number assigned to every healthcare provider. It’s usually printed near the prescriber’s name.
- Prescription number-This is how the pharmacy tracks your script. You’ll need it when you call to refill.
- Pharmacy’s full legal name-Not just “CVS” or “Walgreens.” It should include the exact store location, like “CVS Pharmacy #1234, Main Street, Springfield.”
- Pharmacy phone number-This isn’t a toll-free number. It’s the direct line to the pharmacy where you picked up the medicine.
- Pharmacist’s name-Required in 42 states. If it’s not there, ask why.
These aren’t suggestions. They’re federal and state requirements. If you’re missing any of these, the label is incomplete-and that’s a red flag.
How to Verify the Prescriber Information
Start with the prescriber’s name. Look at it. Say it out loud. Does it match the person who treated you?
Here’s a real example: A patient in Ohio picked up a painkiller labeled as prescribed by their primary care doctor. But they hadn’t seen that doctor in six months. They’d recently visited a dentist for a root canal. The dentist had prescribed the medication, but the pharmacy system auto-filled the wrong provider name. The label said “Dr. Lisa Wong,” but the actual prescriber was “Dr. Mark Chen.”
The patient noticed the mismatch. Called the pharmacy. Turned out the prescription had been sent electronically from the dentist’s office, but the system pulled the wrong NPI number. If the patient hadn’t checked, they could’ve taken a drug that didn’t match their medical history.
Don’t assume the system got it right. Electronic prescriptions are convenient, but they’re also prone to errors. A 2023 report from the Agency for Healthcare Research and Quality found that 18% of labeling errors came from auto-filled prescriber data.
Use this simple three-step check:
- Look at the prescriber name. Is it the person you saw?
- Check the NPI number. You can look it up on the NPPES public database (no login needed) if you’re unsure.
- Compare the specialty. Did your cardiologist prescribe this? Or did it come from a dermatologist? Mismatches here can mean the wrong drug was filled.

Verifying the Pharmacy Details
Now, turn to the pharmacy info. The name should be the exact legal name of the location you picked it up from. If you got it from a CVS in Boston, the label shouldn’t say “Walgreens” or “Pharmacy Services Inc.”
Check the phone number. Is it the one you called when you picked it up? Try calling it. If it rings to a different location-or goes to voicemail with a message that doesn’t match the pharmacy name-something’s wrong.
Also, look for the prescription number. This number should match the one you received when you dropped off the script. If it’s different, the pharmacy might have filled the wrong prescription.
Mail-order pharmacies have a higher error rate than local ones. A 2022 CMS analysis found they make 23% more labeling mistakes than community pharmacies. That’s because they handle more complex, high-volume prescriptions. So if you get your meds by mail, pay extra attention.
When to Verify: Three Critical Moments
You shouldn’t just check the label once. Check it three times:
- When you first get the prescription-Right at the counter. Don’t just grab it and leave. Take 60 seconds to scan the label.
- Before you take the first dose-Even if you’ve taken this drug before, the dosage or prescriber might have changed. Always double-check.
- When you refill-Pharmacies sometimes swap prescriptions during refills. A 2024 ISMP report documented cases where patients received someone else’s medication because the refill system confused similar names.
Patients who verified their labels at all three points reported 27% fewer errors and 31% better adherence to their medication schedules, according to a 2023 PatientPoint survey of 5,000 people.
Common Problems and How to Fix Them
Even with the best systems, mistakes happen. Here are the most common issues-and what to do:
- Misspelled prescriber name-This is the #1 error. “Dr. Smith” instead of “Dr. Smyth.” Ask the pharmacist to spell it out. Most pharmacies keep a printed list of prescriber names for this exact reason.
- Wrong specialty-A dentist prescribed a heart medication? That’s a red flag. Ask the pharmacist to confirm the prescription came from the right provider.
- Small print-If you’re over 65, 37% of you struggle to read the label, according to NIH. Ask for a magnifying glass. Most pharmacies offer them for free.
- Missing pharmacist name-In states where it’s required, this should be there. If it’s not, call the state board of pharmacy. They track compliance.
And don’t be shy about asking questions. Pharmacists are trained to help. One Reddit user in March 2024 shared how they caught a wrong drug because the label said “metformin” but the pill looked different. The pharmacist apologized, checked the batch, and replaced it immediately.
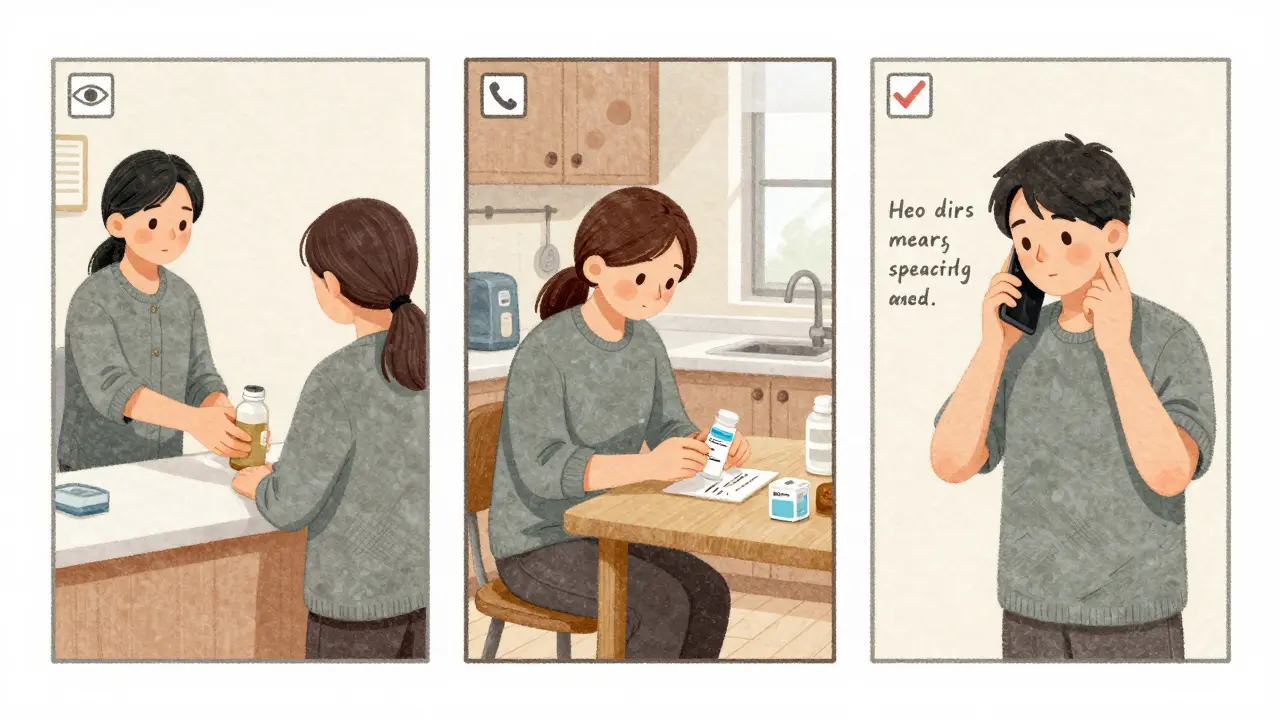
What to Do If You Find an Error
If something doesn’t look right:
- Don’t take the medication.
- Call the pharmacy immediately. Use the phone number on the label.
- Ask to speak to the pharmacist-not just a technician.
- Request a new label with the correct information.
- If they refuse to fix it, contact your prescriber and ask them to reissue the prescription.
In one documented case from May 2023, a patient received a Schedule II opioid prescribed by a dentist, but the label listed a primary care physician. The patient didn’t take it. They called the pharmacy. It turned out someone else’s prescription had been accidentally sent to their account. If they’d taken it, they could’ve been at risk for overdose.
Reporting errors helps fix systems. The FDA’s Adverse Event Reporting System (FAERS) relies on patient reports. If you spot a mistake, report it. It could prevent someone else from getting hurt.
Tools to Help You Stay Safe
You don’t have to do this alone. Many pharmacies now offer tools to help:
- Personal Medication Record (PMR)-Most major chains (CVS, Walgreens, Rite Aid) offer free digital PMRs in their apps. Update it every time you get a new prescription. Use it to compare what’s on the label with what you expect.
- Magnifiers and large-print labels-Ask for them. Over 80% of pharmacies provide them at no cost.
- QR codes-The FDA started a pilot in May 2024 testing QR codes on labels that link to digital verification pages. Early results show a 19% improvement in accuracy. Not widely available yet, but coming.
Still, don’t rely only on apps. A 2023 study in the Journal of the American Pharmacists Association found physical label checks had a 2.1% error rate. Mobile app checks? 7.2%. The screen can glitch. The app can lag. The paper label won’t.
Why This Still Matters in the Digital Age
You might think: “Why bother checking the label when my app says it’s right?”
Because technology isn’t perfect. Systems get confused. Names get swapped. Prescriptions get misrouted.
The FDA’s 2024 report says prescriber verification reduces medication errors by 32% when done consistently. That’s not a small number. That’s life-saving.
Even the American Medical Association warns that relying only on labels can create a false sense of security. Some labels are technically correct but still contain dangerous errors-like the wrong dosage or a drug that interacts with your other meds.
That’s why verification isn’t just about checking names. It’s about being engaged. It’s about asking: “Does this make sense for me?”
And if the answer is no-speak up. You’re not being difficult. You’re being smart.


Melodie Lesesne
January 17, 2026 AT 14:55Also, ask for the big print labels. They're free. No shame.
john Mccoskey
January 18, 2026 AT 02:31Joie Cregin
January 18, 2026 AT 08:02Rob Deneke
January 19, 2026 AT 01:34Pharmacies are busy. They make mistakes. You're not being annoying. You're being alive.
kanchan tiwari
January 19, 2026 AT 17:46Allen Davidson
January 19, 2026 AT 22:17Ryan Hutchison
January 20, 2026 AT 16:51Samyak Shertok
January 22, 2026 AT 06:10But sure. Keep checking labels. Meanwhile, the real problem? The FDA, Big Pharma, and the fact that your doctor gets paid more to prescribe than to listen.
Stephen Tulloch
January 22, 2026 AT 16:24Corey Sawchuk
January 23, 2026 AT 09:28Bobbi-Marie Nova
January 24, 2026 AT 06:02So yeah. Check the label. It's not annoying. It's your superpower.