Every year, thousands of people end up in the emergency room because they took a herbal supplement with their prescription medication-often without realizing it could be dangerous. It’s not just about taking too much. Sometimes, even a daily ginkgo capsule or a bottle of St. John’s Wort can turn a safe drug into a risky one. The problem isn’t the supplement itself. It’s the hidden interaction. And most people have no idea it’s happening.
Why Herbal Supplements Can Be Risky with Prescription Drugs
Herbal supplements aren’t regulated like prescription drugs. That means they don’t have to prove safety or effectiveness before hitting store shelves. Under the Dietary Supplement Health and Education Act of 1994, companies can sell anything labeled as a ‘dietary supplement’ without FDA approval. The agency can only step in after someone gets hurt. That’s why you’ll find products claiming to boost memory, lower blood pressure, or lift your mood-with no warning labels about what they might do when mixed with your heart medication or antidepressant.
The body processes herbs and drugs through the same pathways. Many herbs affect liver enzymes-especially CYP3A4 and CYP2C9-that break down medications. If an herb slows down these enzymes, your drug builds up in your system and can cause toxicity. If it speeds them up, your drug gets cleared too fast and stops working. This isn’t theory. It’s been proven in clinical trials.
Top 5 Dangerous Herbal Interactions
Some herbs are far more likely to cause harm than others. Here are the five with the strongest evidence and the most serious outcomes:
- St. John’s Wort and antidepressants: This herb is one of the most dangerous combinations. It can slash the levels of SSRIs like sertraline and fluoxetine by 20-40%, making them useless. Worse, it can trigger serotonin syndrome-a potentially fatal condition marked by high fever, muscle rigidity, confusion, and rapid heartbeat. The American Academy of Family Physicians says it should be avoided entirely with any antidepressant.
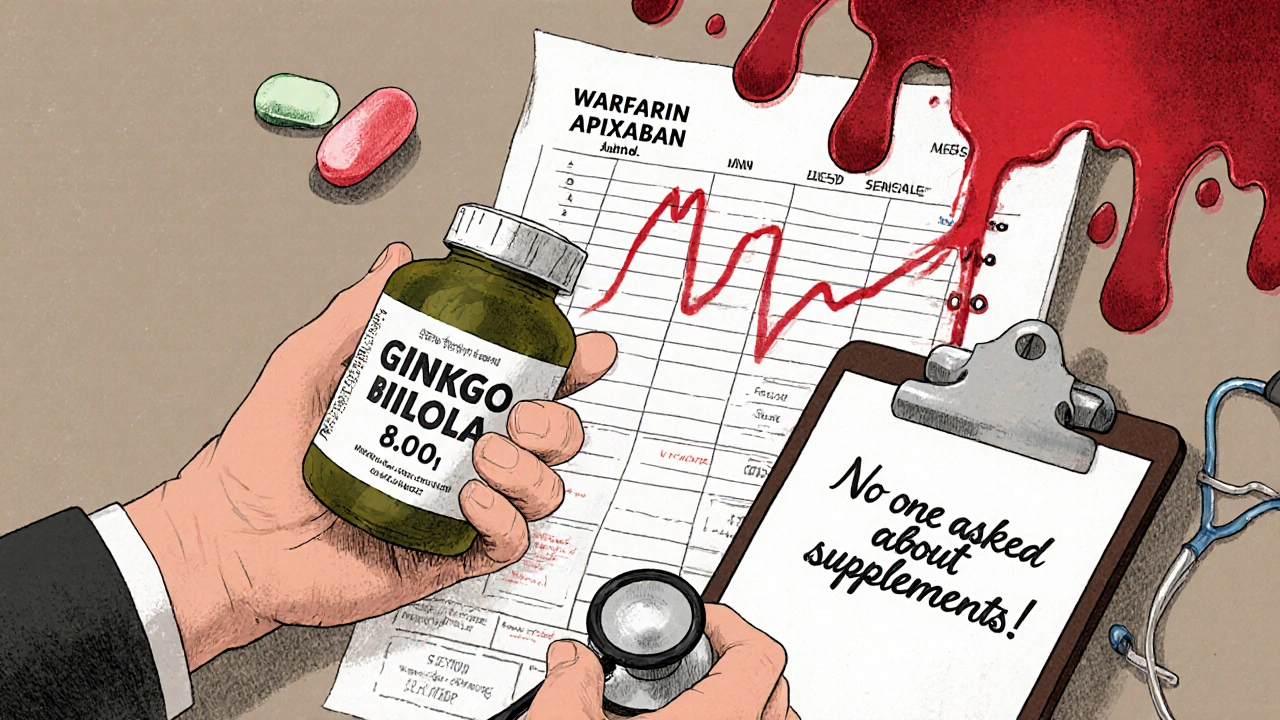
- Ginkgo biloba and blood thinners: Ginkgo is popular for memory and circulation, but it increases bleeding risk. When taken with warfarin, apixaban, or aspirin, it can cause internal bleeding. Mayo Clinic recorded 23 major hemorrhage cases between 2010 and 2020, including three deaths. INR levels can spike above 8.0, far beyond the safe range of 2.0-3.0.
- Garlic supplements and HIV medications: Garlic reduces the concentration of saquinavir, an HIV protease inhibitor, by 51%. That’s enough to let the virus rebound. It also interacts with blood thinners and can increase bleeding risk.
- Goldenseal and many prescription drugs: Goldenseal blocks the CYP3A4 enzyme, which handles about half of all medications. It can raise levels of statins, sedatives, and immunosuppressants like cyclosporine to toxic levels. One study showed a 40% drop in midazolam clearance-meaning sedatives last longer and can cause dangerous drowsiness.
- Coenzyme Q10 and warfarin: Many people take CoQ10 for heart health or statin side effects, but it can reduce warfarin’s effect by 25-30%. That means your blood clots faster. Weekly INR checks are needed if you’re taking both.
What About the ‘Safe’ Herbs?
Not all herbs are equally risky. Some, like milk thistle, saw palmetto, and American ginseng, have little to no documented interaction with common drugs. But that doesn’t mean they’re harmless. The evidence is often weak because most studies are small, short-term, or based on lab results-not real patients.
Cranberry juice is a good example. For years, people were told it could boost warfarin’s effect and cause bleeding. But recent reviews show mixed results. Some studies found no effect. Others saw INR increases in just 12% of users. The inconsistency means doctors can’t give a blanket warning-but they also can’t say it’s safe. If you drink cranberry juice daily and take warfarin, get your INR checked more often.
Even herbs marketed as ‘natural’ or ‘gentle’ can be risky. Chamomile, for example, is often used for sleep or anxiety. But it can interact with sedatives and blood thinners. And if you’re on a beta-blocker for high blood pressure, hawthorn can push your blood pressure too low-leading to dizziness, fainting, or falls.
Who’s Most at Risk?
Older adults are the most vulnerable. Nearly 70% of people over 65 take at least one supplement, and more than half are on two or more prescription drugs. Many don’t realize their supplements are part of their medication list. A University of Michigan study found 76% of supplement users believed ‘natural means safe.’ Only 25% tell their doctor about what they’re taking.
That’s a problem because doctors don’t ask. Most primary care visits focus on symptoms, not supplements. Pharmacists are better trained to catch these interactions, but they’re not always consulted. In the Medicare population, 14.4% of seniors used herbal supplements alongside prescription drugs. Of those, nearly 400 cases involved dangerous bleeding risks from ginkgo, garlic, or ginseng combined with blood thinners.
People on immunosuppressants after organ transplants are also at extreme risk. St. John’s Wort can drop cyclosporine levels by 50-60% in just two weeks. That’s enough to cause organ rejection. One patient lost a kidney transplant because they started taking St. John’s Wort for ‘depression’ without telling their transplant team.
What You Should Do
If you take any prescription medication, here’s what you need to do:
- Make a complete list of everything you take: pills, capsules, teas, tinctures, and even topical creams. Don’t leave out ‘natural’ products.
- Bring it to every doctor and pharmacist visit. Don’t wait to be asked. Say: ‘I take these supplements. Are they safe with my meds?’
- Check high-risk products. If your supplement contains ginkgo, St. John’s Wort, garlic, goldenseal, or licorice, assume it’s risky until proven otherwise.
- Watch for warning signs. Unexplained bruising, nosebleeds, dizziness, confusion, rapid heartbeat, or sudden mood changes could signal a dangerous interaction.
- Use trusted resources. The National Center for Complementary and Integrative Health (NCCIH) has a free, updated herb-drug interaction checker. Memorial Sloan Kettering’s database is also reliable.
Pharmacists can run your list through Stockley’s Herbal Interactions database. It flags interactions by severity: ‘Life-threatening,’ ‘Significant,’ or ‘Moderate.’ Ask them to run your meds and supplements through it. It takes less than five minutes.
The Bigger Problem: Lack of Evidence and Regulation
Here’s the uncomfortable truth: We don’t know enough. Only 15% of documented herb-drug interactions have strong evidence from randomized trials. The rest come from case reports, animal studies, or lab tests. That means some warnings are based on a single patient’s story-not solid science.
But that doesn’t mean you should ignore them. When the stakes are bleeding, organ rejection, or serotonin syndrome, you don’t wait for perfect data. You assume risk until proven safe.
The FDA doesn’t test supplements before they’re sold. Companies don’t have to report side effects unless they’re severe. An estimated 95% of adverse events go unreported. In 2022, the FDA warned 17 companies for slipping actual drugs-like sildenafil or steroids-into their ‘natural’ products. That’s not a supplement issue. That’s a fraud issue.
What’s Changing?
Things are slowly improving. The NCCIH updated its interaction database in January 2024, adding new findings like green tea reducing the effectiveness of the cancer drug bortezomib. Epic Systems, the electronic health record platform used by most U.S. hospitals, plans to integrate NCCIH data into medication reconciliation by late 2025. That means when you’re admitted, your list of supplements could automatically flag interactions.
But until then, the responsibility falls on you. No one else is checking. No one else is asking. If you’re on warfarin, antidepressants, statins, or immunosuppressants, your herbal supplement might be quietly undoing your treatment-or making you sick.
‘Natural’ doesn’t mean safe. And ‘over-the-counter’ doesn’t mean harmless. The only way to stay safe is to talk to your doctor-every time.
Can I take ginkgo biloba if I’m on blood thinners?
No. Ginkgo biloba increases bleeding risk when taken with warfarin, apixaban, rivaroxaban, or aspirin. It can cause internal bleeding, including brain hemorrhages. Studies show it triples the risk of bleeding compared to blood thinners alone. If you’re on any anticoagulant, avoid ginkgo completely.
Does St. John’s Wort affect birth control?
Yes. St. John’s Wort reduces the effectiveness of oral contraceptives by 15-30%, increasing the risk of unintended pregnancy. A 2022 analysis of user reports found 42% of cases involving contraceptive failure led to pregnancy. If you’re on birth control, avoid St. John’s Wort.
Is it safe to take CoQ10 with warfarin?
It can be, but only with close monitoring. CoQ10 reduces warfarin’s effect by 25-30%, which means your blood may clot faster. If you take both, get your INR checked weekly for the first month, then every two weeks. Don’t start or stop CoQ10 without talking to your doctor.
Can I take garlic supplements if I’m on statins?
Garlic supplements may increase the risk of muscle damage when taken with statins. While the interaction isn’t as strong as with blood thinners, garlic can affect liver enzymes that process statins. If you’re on a statin and want to take garlic, stick to dietary garlic (in food) and avoid concentrated supplements unless approved by your doctor.
Why don’t my doctors ask about supplements?
Most doctors don’t ask because they’re not trained to. Medical schools rarely teach herb-drug interactions. Even though 50% of U.S. adults use supplements, many providers assume patients won’t mention them-or don’t think they matter. That’s why you need to bring up supplements yourself. Don’t wait to be asked.


shubham seth
November 17, 2025 AT 09:40Bro this post is a masterclass in fearmongering wrapped in pseudo-science. Ginkgo causes bleeding? So does sneezing too hard. The FDA doesn’t regulate supplements? Neither do they regulate your morning coffee, but nobody’s dropping dead from lattes. You’re acting like every herb is a landmine when most are just… plants. Chill.
Shannon Hale
November 18, 2025 AT 17:03OMG I CAN’T BELIEVE YOU’RE STILL BUYING THIS GARBAGE. St. John’s Wort and SSRIs?? That’s not a ‘risk’-that’s a suicide pact disguised as wellness. I had a friend who took it with Zoloft and ended up in the ER with serotonin syndrome-she had to get a feeding tube because she couldn’t stop shaking. And you think ‘natural’ means safe? Natural means ‘untested by anyone who cares if you live or die.’
Leslie Douglas-Churchwell
November 19, 2025 AT 06:43Let me guess-the pharmaceutical industry paid you to write this. 😏 They’ve been suppressing herbal medicine since the 1930s because it’s cheaper than pills. St. John’s Wort? It’s been used for centuries in Germany to treat depression-better than SSRIs, no side effects. The FDA? A puppet of Big Pharma. They only ‘step in’ when a drug kills 10,000 people… then they charge $500 for the antidote. 🤡
CoQ10 reduces warfarin? Of course it does-it’s a natural anticoagulant modulator! But they’ll never tell you that because it’s not patentable. Wake up, sheeple. 🌿💊
Deb McLachlin
November 19, 2025 AT 20:39While I appreciate the thoroughness of this overview, I must emphasize the methodological limitations inherent in many of the cited case studies. The majority of herb-drug interaction data derive from in vitro models or anecdotal reports, which lack the statistical power to establish causal relationships. For instance, the claim that garlic reduces saquinavir concentrations by 51% originates from a single-phase pharmacokinetic trial with a cohort of n=12. Until randomized controlled trials with clinically relevant endpoints are published, we risk overestimating risk and underestimating patient autonomy. Furthermore, the conflation of ‘unregulated’ with ‘dangerous’ is logically unsound-many over-the-counter NSAIDs carry greater documented risks than most herbal supplements.
Holli Yancey
November 20, 2025 AT 12:39I’ve been on blood thinners for 8 years and take turmeric and omega-3s daily. My INR is always in range. My doctor knows about it. We check every 4 weeks. It’s not about fear-it’s about communication. I get scared reading posts like this because they make people panic and quit things they need. Please don’t scare people into silence. Talk to your provider. That’s the real solution.
saurabh lamba
November 21, 2025 AT 17:10so like… is life just a series of tiny poisonings we don’t notice? 🤔
we eat food grown with chemicals, drink water with fluoride, breathe air with microplastics…
but if i take a ginkgo pill? oh nooooo the apocalypse.
we’re all just lab rats in a capitalist soup.
maybe the real danger is believing we can control everything with pills and warnings.
maybe we should just… live? 🌱
Kiran Mandavkar
November 22, 2025 AT 19:43What’s truly pathetic is how people treat herbal medicine like a hobby while ignoring that every single pharmaceutical drug was originally derived from a plant. You’re not ‘natural’-you’re just ignorant. St. John’s Wort? It’s hyperforin inhibiting CYP3A4-same mechanism as grapefruit juice, which everyone drinks without panic. Why is one ‘dangerous’ and the other ‘normal’? Because the pharmaceutical lobby owns the narrative. Your fear is manufactured. Your trust in Big Pharma? That’s the real drug.
Eric Healy
November 24, 2025 AT 08:49you say ginkgo causes bleeding but you dont say how much you need to take for that to happen. 120mg? 1000mg? 5g? its like saying water causes drowning. also why no data on how many people take these and dont die? 100 million people take ginkgo. 23 cases in 10 years? thats less than 1 in 4 million. you’re scaring people over lottery odds
Jessica Healey
November 26, 2025 AT 02:59my grandma took garlic pills with her blood thinner for 12 years. never had a problem. then she stopped because some blog told her to. and guess what? her cholesterol went through the roof. now she’s on a statin and her liver is fried. so who’s the real villain here? the supplement? or the fear?
Kelsey Robertson
November 27, 2025 AT 04:31Wait-so the fact that the FDA doesn’t regulate supplements is a problem… but the fact that they regulate drugs into $500-a-pill monopolies isn’t? You’re blaming the supplement industry for not being pharmaceuticals… while ignoring that pharmaceuticals are the only things that can legally be patented and priced into oblivion. This isn’t about safety-it’s about control. You’re not warning people-you’re defending a broken system.
Levi Hobbs
November 29, 2025 AT 03:06I really appreciate this breakdown. I work in a pharmacy and we get this question every day. The biggest issue isn’t the herbs-it’s that patients don’t tell us. I had a guy on warfarin take ginseng for ‘energy’ and his INR dropped to 1.1. He didn’t think it mattered. We flagged it, adjusted his dose, and now he brings his supplement list every time. Just talk to someone. It’s that simple.
henry mariono
November 29, 2025 AT 12:02I’m a transplant patient. I take cyclosporine. I was told not to touch St. John’s Wort. I didn’t. I also don’t take any supplements unless my team approves them. I know the stakes. I’m not scared-I’m careful. And I don’t post about it. I just live.
Sridhar Suvarna
November 29, 2025 AT 15:31Let us not forget that in Ayurveda and Traditional Chinese Medicine, herbs are never taken in isolation. They are balanced with diet, lifestyle, and intention. The modern reductionist approach of isolating one herb and calling it dangerous ignores centuries of holistic practice. Perhaps the problem is not the herb-but the context in which we use it. We treat the body like a machine with buttons to press. Maybe we need to treat it like a garden.
Joseph Peel
November 30, 2025 AT 22:02In Japan, green tea is consumed daily by over 80% of the population. The same catechins that may interfere with bortezomib are present in every cup. Yet there is no epidemic of chemotherapy failure. Context matters. Dose matters. Individual variation matters. Blanket warnings do more harm than good by eroding trust in both conventional and complementary medicine.
Gordon Mcdonough
December 1, 2025 AT 03:37AMERICA IS GETTING WEAK!! WE USED TO JUST TAKE OUR MEDS AND SHUT UP!! NOW EVERYONE’S ON HERBS AND GINKGO AND COQ10 AND THINKING THEY’RE SMARTER THAN DOCTORS?? I’M ON 7 PRESCRIPTIONS AND I TAKE NOTHING ELSE!! IF IT’S NOT IN A WHITE PILLS WITH A LABEL IT’S NOT FOR ME!! THIS IS WHY OUR COUNTRY IS FALLING APART!!