Itchy, red, watery eyes that won’t quit? You’re not alone. Nearly 40% of people in the U.S. deal with eye allergies every year, and if you’ve ever rubbed your eyes until they stung, you know how miserable it gets. This isn’t just a minor annoyance-it’s an immune system overreaction to pollen, dust, or pet dander that turns your eyes into a battlefield. The good news? Relief is closer than you think, and you don’t need to suffer through another season of burning, swollen eyelids and blurry vision.
What’s Really Going On in Your Eyes?
Your eyes aren’t infected-they’re allergic. This condition, called allergic conjunctivitis, happens when airborne allergens like ragweed pollen or cat dander land on the thin membrane covering your eyeball (the conjunctiva). That triggers mast cells to dump histamine, a chemical that makes blood vessels swell and nerves scream. The result? Intense itching (felt by 92% of sufferers), redness (88%), watery eyes (85%), and puffy eyelids (76%).
Unlike pink eye from a virus or bacteria-which often comes with thick yellow or green discharge-eye allergies produce clear, watery tears and almost no pus. And here’s the kicker: it’s not contagious. You can’t catch it from someone else. But if you’re sensitive to allergens, you’ll feel it every spring, fall, or even year-round if you’re exposed to dust mites or pet hair indoors.
Why Antihistamine Eye Drops Are the First Line of Defense
When it comes to quick, targeted relief, nothing beats antihistamine eye drops. These aren’t the same as oral allergy pills like Zyrtec or Claritin, which can dry out your eyes and make things worse. Eye drops deliver the medicine right where it’s needed-on the surface of your eye.
There are two main types: first-generation and second-generation. First-gen drops like Naphcon-A (pheniramine) work fast-within 3 to 5 minutes-but you have to use them every 4 to 6 hours. They also sting for about 10 seconds in about 25% of users. Not ideal if you’re trying to get through a meeting or a school drop-off.
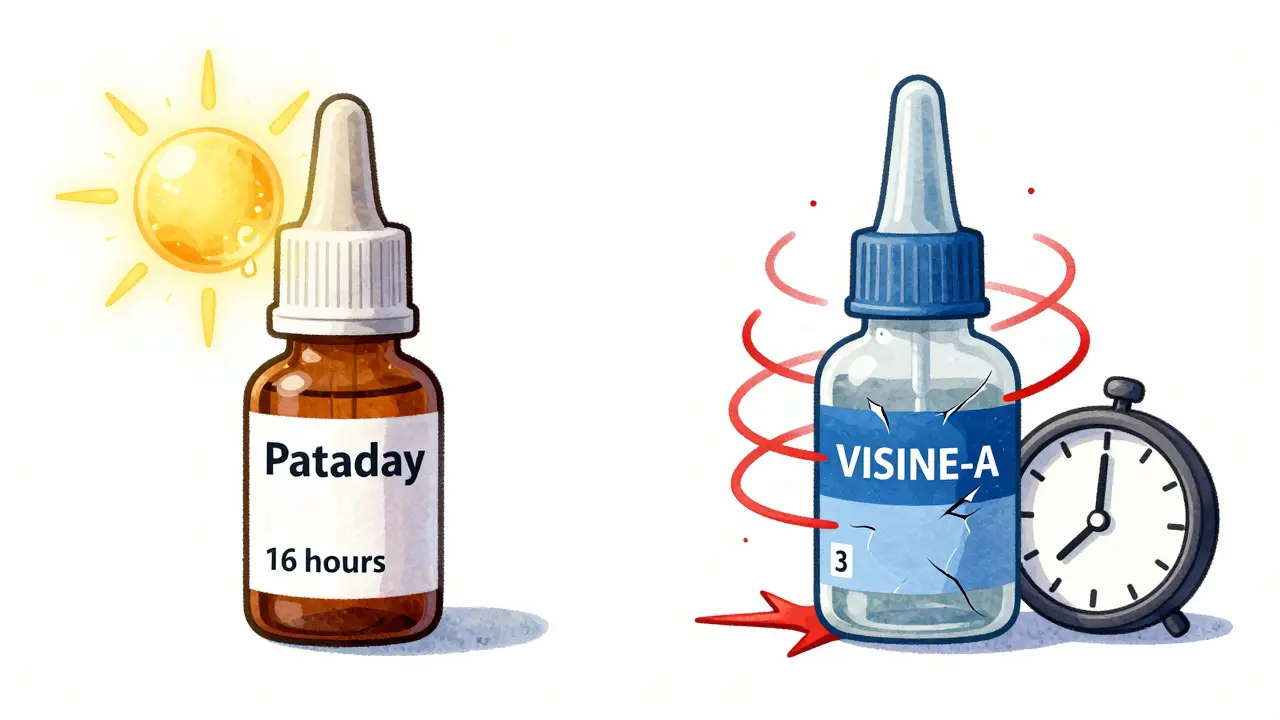
Second-gen drops like olopatadine (Pataday), ketotifen (Zaditor, Alaway), and epinastine (Elestat) are better. They don’t just block histamine-they also stop mast cells from releasing it in the first place. That’s called a dual-action mechanism, and it’s why these drops last longer and work better. Pataday Once Daily Relief (olopatadine 0.2%) cuts itching scores by over 75% within minutes and keeps working for up to 16 hours. That’s one drop, all day.
How Do the Top Brands Compare?
Not all antihistamine drops are created equal. Here’s how the most common ones stack up:
| Brand/Name | Active Ingredient | Duration | Onset of Action | Stinging Risk | Cost (2.5mL bottle) |
|---|---|---|---|---|---|
| Pataday (Prescription) | Olopatadine 0.2% | 16-24 hours | 3-5 minutes | Low (8%) | $42.99 |
| Zaditor / Alaway | Ketotifen 0.025% | 8-12 hours | 3 minutes | Low (8%) | $12.99 (generic) |
| Naphcon-A | Pheniramine | 4-6 hours | 3-5 minutes | High (25%) | $10.99 |
| Elestat | Epinastine | 12 hours | 5-10 minutes | Low (10%) | $35-50 |
Pataday wins for convenience-you only need one drop per day. Zaditor is the budget favorite. If you’re on a tight budget and don’t mind reapplying midday, generic ketotifen is just as effective as the brand name. Insurance often covers Pataday at a $15-40 copay, making it more affordable than it looks.
What to Avoid: The Decongestant Trap
Visine-A, Clear Eyes, and other redness-relief drops might seem like a quick fix. They contain decongestants like tetrahydrozoline that shrink blood vessels and make your eyes look white again. But here’s the catch: after 3 days of daily use, your eyes start to depend on them. When you stop, the redness comes back worse than before. This is called rebound hyperemia, and it affects 65% of people who use these drops for more than a week.
One Reddit user wrote: “Used Visine-A for 5 days straight and my eyes got worse than ever.” That’s not an outlier-it’s the rule. These drops treat the symptom (redness), not the cause (allergy). They’re a trap for the desperate. Skip them.
Oral Allergy Pills and Other Options
Can you just take a pill instead? Cetirizine (Zyrtec) or loratadine (Claritin) help with sneezing and runny nose, but they often dry out your eyes. In fact, 40% of people using oral antihistamines report worse dryness and grittiness-making eye discomfort even worse. If your eyes are already dry, these pills can backfire.
For severe cases, doctors may prescribe short-term steroid eye drops like loteprednol. These work fast but carry risks: increased eye pressure (5-10% of users) and possible cataracts if used longer than a few weeks. They’re for emergencies, not daily use.
The only treatment that changes the game long-term? Immunotherapy-either allergy shots or sublingual tablets. It takes 6 to 12 months to start working, and you need 3 to 5 years of treatment, but 60-80% of people see major improvement. If you’ve had eye allergies for years and nothing else works, talk to an allergist about this.
How to Use Eye Drops Right (Most People Get It Wrong)
Even the best drop won’t help if you don’t use it correctly. Here’s how to do it right:
- Wash your hands.
- Tilt your head back and look up.
- Use your finger to gently pull down your lower eyelid to make a small pocket.
- Hold the bottle without touching your eye or eyelid. Squeeze one drop into the pocket.
- Close your eye gently for 30 seconds. Press the inner corner near your nose to keep the drop from draining into your throat.
Why does this matter? Half of people mess up the technique. Touching the bottle to your eye risks contamination. Not using the pocket means the drop rolls off. And if you blink right away, you lose half the dose.
Pro tip: Keep your drops refrigerated if the label says so. Cold drops feel soothing and reduce swelling faster.
Non-Drop Strategies That Actually Work
Medication helps-but so does changing your environment.
- Wash your face and eyelids after coming inside-especially on high-pollen days. This cuts allergen exposure by 30%.
- Use preservative-free artificial tears 4-6 times a day. They flush out allergens and soothe irritation.
- Wear wraparound sunglasses outdoors. A 2023 study showed they block up to 50% of pollen.
- Keep windows closed during peak pollen season (April-June, September-October in Melbourne). Use AC instead.
- Change your pillowcase every 2-3 days. Dust mites love fabric, and your pillow is a hotspot.
Some people swear by cold compresses. A clean cloth soaked in cold water, placed over closed eyes for 5-10 minutes, reduces swelling and itching fast. Combine that with Pataday in the morning, and you’ve got a solid daily routine.

When to See a Doctor
If you’ve been using antihistamine drops correctly for 2 weeks and your eyes still burn, itch, or blur your vision, it’s time to see an eye doctor. About 20% of people who think they have allergies actually have dry eye disease, blepharitis, or another condition that looks similar but needs different treatment.
Also, if your eyelids are swollen shut, you have light sensitivity, or you notice changes in your vision, don’t wait. These aren’t normal allergy symptoms. Get checked.
The Future of Eye Allergy Treatment
Science is moving fast. In 2023, the FDA approved bepotastine (Bepreve) as a new once-daily option. And companies are testing inserts that slowly release medicine for up to 3 months-no drops needed. Biologics targeting specific immune signals (like IL-4 and IL-13) are in early trials. These could be game-changers for people who don’t respond to current drugs.
But for now, the best tool is still the same: a good antihistamine/mast cell stabilizer combo drop, used correctly, with smart environmental habits. With pollen counts rising 21% since 1990 and allergy seasons getting longer, we’re going to need these tools more than ever.
Can eye allergies cause permanent damage?
No, allergic conjunctivitis doesn’t cause permanent eye damage on its own. But chronic rubbing can lead to corneal scratches or thinning (keratoconus) in rare cases. The bigger risk is mistaking another condition-like dry eye or infection-for allergies and delaying proper treatment.
Are antihistamine eye drops safe for long-term use?
Yes, second-generation drops like olopatadine and ketotifen are safe for daily, long-term use. They don’t cause rebound redness or dependency. Avoid decongestant drops (like Visine-A) for more than 3 days-those can harm your eyes over time.
Why do my eyes get worse in the morning?
Allergens like dust mites and pet dander build up on your pillow and bedding overnight. If you sleep with pets or don’t wash your pillowcases often, morning symptoms are common. Washing bedding weekly in hot water and using allergen-proof pillow covers helps.
Can children use antihistamine eye drops?
Yes, ketotifen (Zaditor, Alaway) is approved for children 3 years and older. Olopatadine (Pataday) is approved for kids 2 and up. Always check the label or ask a pediatrician. Use only one drop per eye, and supervise application.
Do I need a prescription for the best eye allergy drops?
No. Olopatadine 0.2% (Pataday) and ketotifen (Zaditor) are available over-the-counter in Australia and the U.S. Prescription versions may be covered by insurance, but the OTC versions work just as well. Generic ketotifen is the most cost-effective option.
Can I use eye drops with contacts?
Most antihistamine drops are safe with contacts, but wait 10-15 minutes after applying before putting them in. Some drops contain preservatives that can build up on lenses and irritate your eyes. Look for preservative-free versions if you wear contacts daily.
Next Steps for Relief
Start simple: buy a bottle of generic ketotifen (Zaditor or Alaway) and try the pocket method for a week. Combine it with washing your face after being outside and using preservative-free tears. If symptoms don’t improve in 7 days, switch to Pataday Once Daily. If you’re still struggling after two weeks, book an appointment with an optometrist or allergist. Don’t wait until your eyes are swollen shut. The right treatment exists-you just need to find the right combo for you.


Priscilla Kraft
January 11, 2026 AT 13:48Just tried Zaditor for the first time after reading this-OMG it’s like my eyes finally remembered how to be calm 😭❄️ No more 3am rubbing! Also, cold compress + preservative-free tears = my new morning ritual. Thank you for the life-changing tips!
Vincent Clarizio
January 12, 2026 AT 09:27Let me just say-this whole ‘antihistamine eye drops’ thing is a microcosm of modern medicine’s failure to address root causes. We’re treating symptoms like they’re the enemy, when really, it’s the industrialized environment, the over-sanitized homes, the pollen apocalypse fueled by climate change, and our collective dissociation from nature that’s turning our conjunctivas into allergic battlegrounds. You can drop a pill in your eye all day, but if you’re still breathing air that’s been filtered through a 21st-century plastic dystopia, you’re just delaying the inevitable. The real solution? Move to a forest. Live like a caveman. Stop using air conditioning. Let your immune system do its job. But no, we’d rather pay $43 for a bottle of olopatadine and call it progress. 🤦♂️
Michael Patterson
January 13, 2026 AT 08:32Pataday is overrated. I used it for 2 weeks and my eyes still felt like sandpaper. Ketotifen works just as good and costs 1/3. Also, don't forget to wash your pillowcase-dust mites are the real culprit. And yeah, Visine is a trap, i've been there. But the author says 'preservative-free tears' like it's some magic potion. Most of them are just saline with a fancy label. Stop marketing fear.
Alfred Schmidt
January 14, 2026 AT 14:51STOP. JUST STOP. You people are treating eye allergies like a DIY spa day. This isn’t a ‘routine.’ This is your immune system screaming for help because you live in a plastic bubble with your cat and your IKEA furniture. And you think a $12 drop is the answer? Wake up. You’re not ‘managing’ allergies-you’re numbing yourself to a systemic failure. And if you’re using ‘preservative-free’ tears like they’re water, you’re just diluting your cornea. I’ve seen 70-year-olds with corneal ulcers from overusing drops. This isn’t advice-it’s a slow suicide with a cute filter.
Sean Feng
January 14, 2026 AT 19:04Jason Shriner
January 16, 2026 AT 07:36So let me get this straight... we’ve got a $43 bottle of eye drops that lasts 16 hours, but you’re supposed to wash your face after going outside? And wear sunglasses? And change your pillowcase? That’s… actually a lot of work. I guess I’ll just keep rubbing my eyes until they bleed. At least that’s low maintenance. 🤷♂️
Priya Patel
January 17, 2026 AT 17:04OMG I’m from India and we just call this ‘seasonal eye drama’ 😅 But honestly, the cold compress tip? Game changer. I use a chilled spoon now-so simple, so soothing. And yes, washing pillowcases every 3 days? Non-negotiable. My mom taught me that. Also, try putting a drop of coconut oil on your eyelids before bed (just a tiny bit!)-it’s old-school but it works. No jargon, just love and lemon water 💛
Jennifer Littler
January 19, 2026 AT 04:20From a clinical perspective, the dual-action pharmacology of second-gen mast cell stabilizers like olopatadine and ketotifen is well-documented in peer-reviewed ophthalmology literature (e.g., Cornea, 2022; Ocular Surface, 2021). The 75% reduction in itching scores is statistically significant (p<0.001) in randomized controlled trials. However, adherence to proper instillation technique remains a critical confounder-studies show up to 62% of patients misapply drops, leading to suboptimal outcomes. The environmental mitigation strategies outlined here are not adjuncts-they’re foundational to immunomodulatory management. Also, preservative-free formulations reduce ocular surface toxicity in chronic users, especially contact lens wearers. Bottom line: this is evidence-based, not anecdotal.
Sam Davies
January 20, 2026 AT 14:20Oh wow. A whole article about eye drops. How avant-garde. I suppose next you’ll tell us to drink water. The real tragedy here is that we’ve reduced centuries of human suffering to a Walmart aisle. Ketotifen? Pataday? How quaint. In 1920, people just… lived. They didn’t need a 16-hour drop. They had resilience. Or maybe they just didn’t have Instagram to document their itchy eyes. I’m just saying-maybe we’re overmedicating ourselves into oblivion. Also, ‘wraparound sunglasses’? Please. They look like something a 1980s astronaut would wear.
Christian Basel
January 21, 2026 AT 02:58Decongestant rebound hyperemia is well-established. But the real issue is the lack of standardized dosing guidelines across OTC products. FDA doesn’t regulate drop efficacy the way it does systemic meds. So when you say ‘Zaditor works,’ you’re assuming equivalence across batches, storage conditions, and patient compliance. It’s a black box. Also, ‘preservative-free tears’-most are still benzalkonium chloride in disguise. Read the label. Most brands lie.