When your body can’t use sugar for energy, it starts burning fat instead. That sounds harmless-until it turns your blood acidic. That’s diabetic ketoacidosis, or DKA. It doesn’t sneak up. It hits fast. And if you wait too long, it can kill you. This isn’t rare. Every year in the U.S. alone, over half a million people end up in the hospital because of it. Most are young people with type 1 diabetes who didn’t realize their insulin had failed. Others are adults with type 2 who skipped doses during illness. Either way, the clock starts ticking the moment symptoms appear.
What Happens When DKA Starts
Your body needs insulin to move glucose from your blood into your cells. Without it, glucose builds up-sometimes over 500 mg/dL. But your cells are starving. So your liver starts breaking down fat for fuel. That process spits out ketones. Ketones are acids. Too many of them, and your blood pH drops. Normal blood pH is 7.35 to 7.45. In DKA, it can crash below 7.1. That’s life-threatening.What makes DKA dangerous isn’t just the high sugar. It’s the combo: high glucose, high ketones, and acid in your blood. You can even have DKA with glucose under 250 mg/dL. That’s called euglycemic DKA, and it’s rising-especially in people using SGLT2 inhibitors like Farxiga or Jardiance. These drugs lower blood sugar by flushing glucose out in urine, but they also increase ketone production. If you’re on one and get sick, your risk jumps.
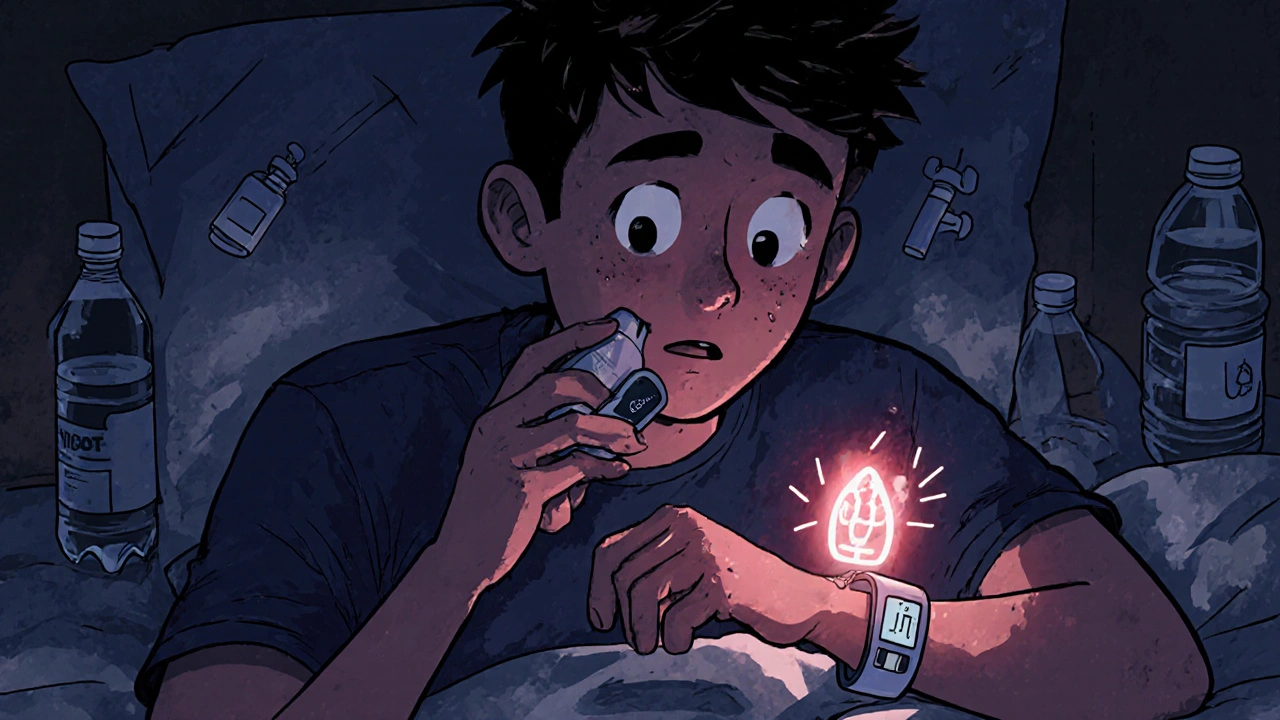
Early Warning Signs You Can’t Ignore
The first signs are easy to miss. You’re thirsty-really thirsty. You’re peeing every hour, even at night. You’ve drained two liters of water and still feel dry. Your mouth feels like sandpaper. That’s not just dehydration. That’s your body trying to flush out sugar and ketones.Then comes nausea. Not just upset stomach-actual vomiting. About two out of three people with DKA throw up. You might think it’s the flu. But if you’ve got diabetes and you’re vomiting, don’t wait. Check your blood sugar. Check your ketones. If your glucose is over 240 mg/dL and your ketone meter shows moderate or large ketones, you’re in danger.
Abdominal pain is another red flag. It’s sharp, crampy, and often mistaken for appendicitis or food poisoning. In fact, 18% of adult DKA cases are misdiagnosed as gastroenteritis in emergency rooms. If you have diabetes and stomach pain with nausea, assume it’s DKA until proven otherwise.
Extreme fatigue hits hard. You can’t get out of bed. Your muscles feel like lead. Your grip strength drops. You can’t hold a coffee cup. That’s not laziness. That’s your cells starving. Your brain isn’t getting fuel. Your body is shutting down.
The Critical Signs: When You Need an Ambulance
If you’ve had symptoms for 12 to 24 hours, things get serious. Your breathing changes. You start taking deep, fast breaths-25 to 30 per minute. It’s called Kussmaul breathing. Your body is trying to blow off acid by exhaling carbon dioxide. It sounds like panting. It’s not normal.You might smell it before you hear it. A sweet, fruity odor on your breath-like nail polish remover or overripe apples. That’s acetone, a ketone. Clinicians recognize it instantly. If someone says you smell like fruit, don’t laugh. Get checked.
Confusion sets in. You forget your name. You can’t follow a simple conversation. Your eyes glaze over. That’s when your blood pH drops below 7.1. Your brain is drowning in acid. This isn’t just feeling tired. This is neurological damage waiting to happen.
And then, the worst: loss of consciousness. One in seven people admitted to the ICU with DKA are already unconscious when they arrive. That’s not a late-stage symptom. That’s a death sentence if you don’t act.

What Happens in the Hospital
There’s no home treatment for DKA. No pill. No trick. You need IV fluids, insulin, and electrolytes-fast.Within the first hour, you’ll get 1 to 1.5 liters of salt water (0.9% sodium chloride) through an IV. This isn’t just hydration. It’s flushing out ketones and restoring blood flow to your organs. After that, fluids slow to 250-500 mL per hour. Too fast, and you risk brain swelling-especially in kids.
Insulin starts immediately. A small IV bolus, then a continuous drip at 0.1 unit per kilogram per hour. Your blood sugar should drop 50-75 mg/dL per hour. Too fast? You can trigger cerebral edema. Too slow? The acid keeps building. It’s a tightrope.
Ketones are tracked every 2-4 hours. Blood ketone meters are now standard in ERs. Urine strips? Outdated. Blood tests are accurate and fast. You’re not discharged until your ketones are under 0.6 mmol/L, your bicarbonate is above 18, and your pH is back above 7.3-on two tests.
Electrolytes are a silent killer. Your potassium looks normal on the first blood test. But you’re dangerously low inside your cells. Insulin pushes potassium into cells. So your serum level drops fast. You’ll get potassium IV, even if your number looks fine. About 80% of DKA patients need it.
Bicarbonate? Rarely used. Only if your pH is below 6.9. Giving it too early can make things worse. Most hospitals now follow the rule: no bicarbonate unless you’re barely breathing and your blood is nearly pure acid.
What Triggers DKA-and How to Prevent It
Infections are the #1 trigger. Pneumonia, urinary tract infections, even a bad cold. Illness makes your body fight back with stress hormones. Those hormones block insulin. If you’re on insulin, your dose might need to go up during sickness. Many people don’t know that.Insulin omission is next. Missed doses. Running out. Skipping because it’s expensive. In the U.S., the average monthly insulin cost is $374. People ration. They cut doses. They skip. That’s how DKA starts. In Australia, Medicare covers insulin, but out-of-pocket costs still hit hard for some. If you’re struggling to afford your meds, talk to your doctor. There are programs. There are alternatives.
Insulin pumps fail. Infusion sets clog. Tubing kinks. You think you’re covered-but if your pump stops working and you don’t switch to injections, DKA can hit in under 12 hours. Tandem Diabetes Care recommends switching to pens during illness. Always have backup.
New-onset diabetes? One in five DKA cases is the first sign someone has type 1. Kids, teens, even adults in their 30s. They thought they were just tired. They thought the thirst was stress. They didn’t know diabetes could strike out of nowhere.

Technology Is Changing the Game
Continuous glucose monitors (CGMs) are the biggest game-changer. People using Dexcom G7 or Abbott Libre 3 report a 76% drop in DKA episodes. Why? Because they get alerts. High glucose. Rising ketones. Even before symptoms start.Some CGMs now predict DKA 12 hours in advance. The FDA approved DiaMonTech’s algorithm in 2023. It analyzes trends-how fast glucose is rising, how ketones are climbing-and gives a warning. It’s not perfect. But it’s saving lives.
Emergency departments are catching on too. The American College of Emergency Physicians now requires point-of-care ketone testing for any diabetic with glucose over 250 mg/dL. In pilot programs, missed DKA cases dropped by 37%. That’s huge.
What You Should Do Right Now
If you have diabetes:- Check your blood sugar every 4 hours when you’re sick.
- Test ketones if your glucose is above 240 mg/dL. Use a blood meter, not urine strips.
- If ketones are moderate or large, call your doctor or go to the ER. Don’t wait.
- Never stop insulin-even if you’re not eating. Adjust dose, don’t skip.
- Have a sick-day plan. Write it down. Keep it in your phone. Know when to call for help.
- If you’re on an SGLT2 inhibitor, know your risk. Talk to your doctor about ketone testing during illness.
And if you’re caring for someone with diabetes: learn the signs. Know what Kussmaul breathing looks like. Know that fruity breath isn’t just bad hygiene-it’s a warning siren. If they’re vomiting, confused, or lethargic, don’t assume it’s a bug. Assume it’s DKA.
Recovery and Aftercare
Most people stay in the hospital 2.5 to 4 days. If your blood pH was above 7.0, you’ll likely go home in 2 days. Below 7.0? You’re looking at 4 days or more.Going home doesn’t mean you’re done. One in eight people have DKA come back within 72 hours. Why? They stop insulin too soon. They think they’re fine because their glucose dropped. But ketones linger. They need to be fully cleared.
Follow-up is critical. You need to see your endocrinologist within 48 hours. Your insulin regimen might need tweaking. Your pump might need checking. Your triggers need addressing. Was it an infection? Stress? Cost? You can’t just go back to normal. You need a plan.
And if you’ve had DKA once, you’re at higher risk for another. That’s why education matters. Not just about insulin. About recognizing the early signs. About acting before it’s too late.
Can you have DKA without high blood sugar?
Yes. This is called euglycemic DKA. It happens when ketones build up even though blood glucose is below 250 mg/dL. It’s most common in people using SGLT2 inhibitors like Farxiga or Jardiance, especially during illness, fasting, or after reducing insulin. It’s dangerous because it’s easily missed-many assume low sugar means no emergency.
How long does it take for DKA to become life-threatening?
Symptoms can develop in 4 to 12 hours. If untreated, DKA can lead to coma or death within 24 to 48 hours. Delaying treatment by more than 2 hours increases mortality risk by 15% per hour, according to Dr. Irl Hirsch of the University of Washington. The faster you get fluids and insulin, the better your chance of survival.
Is DKA only a problem for people with type 1 diabetes?
No. While 80% of DKA cases occur in type 1 diabetes, it can also happen in type 2 diabetes-especially during serious illness, infection, or when insulin therapy is stopped. People on SGLT2 inhibitors are at higher risk, even if they’re not insulin-dependent. DKA is not exclusive to type 1.
Can I treat DKA at home with extra insulin?
No. DKA requires hospital care. You need IV fluids to rehydrate and flush out ketones. You need precise insulin dosing to avoid dangerous drops in blood sugar or brain swelling. Home insulin injections won’t fix the acidosis or electrolyte imbalance. Delaying hospital care increases death risk. If ketones are moderate or large, go to the ER immediately.
Why do doctors avoid giving bicarbonate for DKA?
Bicarbonate can worsen outcomes. It doesn’t improve survival and may cause brain swelling, low potassium, or paradoxical acidosis in brain tissue. It’s only used if blood pH is below 6.9-rarely needed. Most patients recover fully with fluids and insulin alone. Guidelines from the ADA and ISPAD strongly discourage routine bicarbonate use.
What’s the most common mistake people make during a DKA episode?
Waiting too long. Most people wait 6 hours or more after symptoms start before seeking help. They think it’s the flu, a stomach bug, or that they’ll “just take more insulin.” But DKA progresses fast. By the time nausea, vomiting, or confusion appear, you’re already in crisis. The rule is simple: if you have high blood sugar and moderate/large ketones, go to the hospital-don’t wait.

Bruce Bain
November 19, 2025 AT 05:30Just saw my cousin go through this last year. Thought he had the flu, but his ketones were through the roof. Got to the ER just in time. Don’t wait. Check your numbers. Save your life.
kim pu
November 19, 2025 AT 21:29So let me get this straight-big pharma’s pushing SGLT2 inhibitors because they make people sick, then they sell them the ER visits? 😏 I’ve been on Jardiance for 2 years and my doc never mentioned this. Coincidence? Or profit-driven malpractice? 🤔
Emily Entwistle
November 21, 2025 AT 19:07OMG this is so important!! I just started using my CGM and it beeped at 3am when my ketones spiked. I called my endo and we adjusted my insulin before I even felt sick. 🙏❤️
deepak kumar
November 23, 2025 AT 13:29In India, many diabetics don’t even have access to ketone strips. I’ve seen people use urine strips and wait until they’re vomiting. This post is a lifeline. Please share it with anyone who needs it. 🙏
malik recoba
November 23, 2025 AT 18:53i had no idea euglycemic dka was a thing… my buddy got hospitalized last month with glucose at 180 and ketones at 4.2. doc said he almost didn’t make it. thanks for explaining this so clearly. i’ll make sure my sister knows now.
Duncan Prowel
November 25, 2025 AT 16:24The clinical protocols outlined here are rigorously evidence-based and align with current ADA and ISPAD guidelines. Notably, the avoidance of bicarbonate therapy except in extreme acidosis (pH <6.9) is supported by multiple randomized controlled trials demonstrating no mortality benefit and potential for iatrogenic harm. The emphasis on serial blood ketone monitoring over urine dipsticks reflects a paradigm shift in emergency endocrinology. Furthermore, the aggressive but calibrated fluid resuscitation protocol-avoiding cerebral edema while correcting volume depletion-is a masterclass in risk-benefit balancing. This is precisely the kind of granular, actionable guidance that saves lives in resource-constrained environments.
Dave Pritchard
November 25, 2025 AT 17:13If you’re reading this and you’re scared-don’t be. You’re not alone. DKA is scary, but it’s preventable. Learn the signs. Test your ketones. Have a plan. Talk to your care team. You’ve got this. And if you’re helping someone else? You’re already doing something amazing.
Sameer Tawde
November 27, 2025 AT 13:52Check ketones. Don’t wait. Save your life. Simple. Done.
Jonathan Gabriel
November 28, 2025 AT 05:31So… let me get this straight. You’re telling me that if I’m on Farxiga and get a cold, I’m basically playing Russian roulette with my brain? And the doctors won’t even give me bicarbonate because it’s ‘not proven’? But they’ll give me 4 liters of saline and a 12-hour insulin drip? What if I’m poor and can’t afford a CGM? What if I work two jobs and can’t take off to go to the ER? This isn’t medicine. This is a luxury game where only the rich get to live. 😅
Don Angel
November 29, 2025 AT 09:21Okay, I just read this three times. I’m not a doctor, but I have type 1. And I’ve been so scared of this. Thank you. Thank you. Thank you. I’m printing this out and taping it to my fridge. And I’m telling my mom. And my sister. And my roommate. This needs to be everywhere.
Sarbjit Singh
November 30, 2025 AT 03:01Bro, I lost my cousin to DKA last year. He thought he was fine because his sugar was 'only' 280. He didn't check ketones. He slept it off. He never woke up. Please, please, please test your ketones. Don't be like him. 💔
Angela J
December 1, 2025 AT 16:06Did you know that the FDA approved that ‘predictive algorithm’ for CGMs right after the insulin price hike? Coincidence? Or is this all just a trap to make us buy more expensive tech so they can charge us more for ‘emergency care’? I’ve seen the patterns. They want us dependent. Always watching. Always buying. Always afraid.
benedict nwokedi
December 2, 2025 AT 08:12So… this whole thing is just a corporate propaganda piece disguised as medical advice? SGLT2 inhibitors? CGMs? ‘Guidelines’? All designed to keep us docile, dependent, and paying for ‘solutions’ to problems they created? The real danger isn’t DKA-it’s trusting the system that profits from it. I’m off insulin. I’m fasting. I’m doing keto. And I’m not going to the hospital. Ever.