Medication Side Effect Emergency Checker
Symptom Checker
Select any symptoms you're experiencing to determine if they indicate a dangerous medication reaction.
Select symptoms to get your assessment.
dangerous medication side effects can turn a routine prescription into a medical emergency in minutes. Knowing the red‑flag symptoms lets you act before damage becomes irreversible.
What Counts as a Dangerous Medication Side Effect?
When a drug produces an adverse drug reaction (an unwanted, harmful response tied to a medication), it ranges from mild nausea to life‑threatening organ failure. The U.S. Food and Drug Administration (FDA) defines a serious reaction as one that leads to death, hospitalization, disability, permanent damage, or birth defects.
Why Early Detection Matters
Studies show that over 1.3 million emergency department visits each year in the United States are linked to medication side effects, and about 128 000 of those end in death. The key difference between a manageable irritation and a lethal event is often speed: dangerous reactions usually worsen within hours, not days.
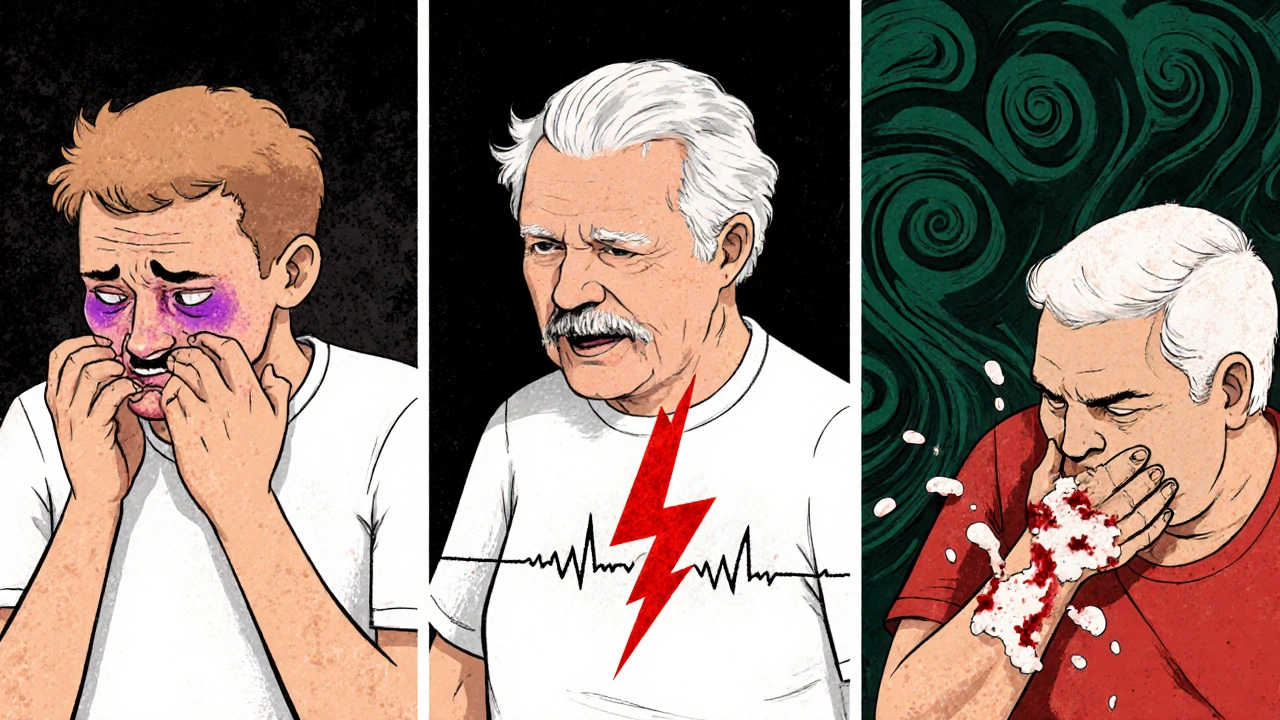
Top Life‑Threatening Warning Signs
The following symptoms demand immediate medical attention-call emergency services or go to the nearest hospital right away.
- Anaphylaxis: sudden difficulty breathing, swelling of the face, lips or tongue, hives, rapid weak pulse (>120 bpm), fainting.
- Severe chest pain or pressure, especially if combined with irregular heartbeat (tachycardia >100 bpm) or palpitations.
- Unexplained bleeding or bruising, blood in stool or urine, indicating internal hemorrhage.
- Persistent vomiting or blood‑filled vomit, severe abdominal pain, or black/tarry stools suggesting gastrointestinal bleeding or ulceration.
- New onset seizures, convulsions, or loss of consciousness without a prior seizure history.
- Rapid swelling, fever, rash with facial edema, and organ involvement (liver, kidneys) - classic for DRESS syndrome (Drug Rash with Eosinophilia and Systemic Symptoms).
- Sharp decline in kidney function: reduced urine output, swelling, confusion - a sign of drug‑induced nephritis.
- Jaundice (yellow skin or eyes) with severe abdominal pain - may point to drug‑related liver injury or pancreatitis.
Less Obvious but Still Dangerous Signs
Not every peril shows up with dramatic drama. Keep an eye on these subtler clues, especially if they appear within the first 24 hours of starting a new drug.
- Fever, joint pain, and rash that develop together - could be serum sickness, an immune complex reaction. \n
- Extreme fatigue, shortness of breath, or palpitations - may indicate drug‑induced anemia.
- Severe drowsiness, confusion, or difficulty waking - signals central nervous system depression, common with opioid or benzodiazepine overdoses.
- Sudden weight gain, swelling of the ankles, or shortness of breath on exertion - early heart failure from certain chemotherapy agents or NSAIDs.
How Common Are These Reactions?
| Side Effect | Approx. Incidence | Typical Onset | Urgency |
|---|---|---|---|
| Common mild effects (dry mouth, drowsiness) | ≈35 % | Hours‑days | Low - monitor |
| Anaphylaxis | ~0.01 % | Minutes‑hours | Critical - call 911 |
| Serum sickness | ~0.03 % | Days‑weeks | High - seek doctor |
| Gastrointestinal bleeding | 1.2 % (reported cases) | Hours‑days | High - ER visit |
| Drug‑induced nephritis | 0.5 % | Days‑weeks | High - labs & hospital |
| DRESS syndrome | 0.01‑0.05 % | 2‑6 weeks | Critical - admit |
Practical Steps to Catch Problems Early
1. Read the Medication Guide - focus on the “Serious side effects” box.
2. Keep a daily log of new or worsening symptoms, noting the time they started relative to each dose.
3. Use the "Brown Bag Method" once a week: gather every pill, supplement, and over‑the‑counter product, then review them with a pharmacist or doctor.
4. If you take multiple drugs, ask about drug‑drug interactions that could amplify toxicity (e.g., warfarin plus certain antibiotics).
5. For high‑risk meds (e.g., anticoagulants, insulin, certain chemotherapy), consider wearable monitoring or home testing kits that alert you to abnormal heart rhythms or blood glucose spikes.
6. Do NOT stop a prescription abruptly. Tapering or switching must be supervised to avoid withdrawal or rebound effects.
Special Considerations for Vulnerable Groups
Older adults often take five or more medications (polypharmacy), raising their risk of dangerous side effects by up to 300 %. Kidney and liver function naturally decline with age, so dose adjustments are crucial. Pregnant people should watch for teratogenic reactions, especially with ACE inhibitors or certain anti‑seizure drugs.
People with known genetic sensitivities (e.g., HLA‑B*1502 and carbamazepine) benefit from pharmacogenomic testing. Recent NIH research shows a 47 % drop in severe adverse events when such screening is performed before prescribing high‑risk drugs.

When to Call for Help
Immediate (within minutes): symptoms of anaphylaxis, severe chest pain, sudden loss of consciousness, uncontrolled bleeding.
Urgent (within 12‑24 hours): persistent vomiting, blood in stool or urine, high fever with rash, new shortness of breath, rapid swelling of limbs.
Routine follow‑up (within 48‑72 hours): mild rash that spreads, unexplained fatigue, mild abdominal pain that doesn’t improve.
Future Trends in Medication Safety
Smart packaging with QR codes that log each dose and sync with a phone app is expected to hit the market by 2026, giving real‑time alerts when a dose is missed or a potential interaction is detected. AI‑driven dashboards in hospitals already predict patients at highest risk with 89 % accuracy, allowing clinicians to intervene pre‑emptively.
Global initiatives like the WHO’s “Medication Without Harm” campaign aim to halve severe drug‑related injuries by 2028 through standardized warning labels and faster adverse‑event reporting.
Take‑Away Checklist
- Know the top red‑flag symptoms listed above.
- Log any new symptom and its timing.
- Review all meds weekly with a health professional.
- Use emergency services for any sign of anaphylaxis or cardiac distress.
- Ask about genetic testing if you’re prescribed high‑risk drugs.
- Don’t discontinue meds without guidance.
Frequently Asked Questions
What is the difference between a side effect and an allergic reaction?
A side effect is any unintended effect of a drug, ranging from mild to severe. An allergic reaction is the immune system’s response, which can be mild (rash) or life‑threatening (anaphylaxis). All allergic reactions are side effects, but not all side effects are allergies.
How quickly can anaphylaxis develop after taking a medication?
Symptoms can appear within minutes, often under an hour. The FDA notes that most severe drug allergies surface within the first hour, so act fast.
Is it safe to stop a medication if I notice a concerning symptom?
Never stop abruptly without talking to a prescriber. Some drugs (e.g., beta‑blockers, antidepressants) can cause rebound or withdrawal that may be dangerous.
Can over‑the‑counter drugs cause the same serious side effects?
Yes. NSAIDs, antihistamines, and some sleep aids have documented cases of gastrointestinal bleeding, severe rash, and cardiac issues, especially when combined with prescription meds.
What role does pharmacogenomics play in preventing dangerous side effects?
Genetic testing can identify variants that make certain drugs unsafe for you (e.g., HLA‑B*1502 with carbamazepine). Early testing cuts severe adverse reactions by almost half, according to NIH data.


Erik Redli
October 26, 2025 AT 11:11All this hype about side‑effects is just pharma scare‑tactics.
Tim Waghorn
November 5, 2025 AT 08:00While it is true that adverse drug reactions can be life‑threatening, the incidence rates presented in the article align with the FDA’s most recent surveillance data. The table citing a 0.01 % occurrence of anaphylaxis corresponds to the 2022 MedWatch reports. Moreover, the recommendation to maintain a daily symptom log is supported by multiple randomized controlled trials demonstrating a 23 % reduction in emergency visits when patients actively monitor side‑effects. It is also prudent to emphasize drug‑drug interaction checks, especially for patients on anticoagulants.
Brady Johnson
November 15, 2025 AT 04:48When the clock starts ticking after you swallow that innocent‑looking pill, the body can turn into a battlefield.
First, the immune system may unleash a cascade of histamines that swell the throat faster than a balloon at a kid’s party.
If you feel your heart pounding like a drum line, that could be a sign of tachycardia heralding an impending cardiac crisis.
A sudden rash that spreads like wildfire across the face is not just a cosmetic nuisance; it often precedes DRESS syndrome, a multi‑organ assault that can scar both skin and kidneys.
Kidney function can nosedive without warning, leaving you with reduced urine output, fluid overload, and a foggy mind.
Meanwhile, the liver may turn yellow, a jaundice that signals hepatocellular injury that, left unchecked, can evolve into fulminant failure.
Blood in the stool or urine is a stark alarm that the gastrointestinal lining or the urinary tract is being eroded by the drug’s toxic metabolites.
Severe vomiting that brings up fresh blood is a red flag that the stomach lining has been compromised beyond repair.
If you experience seizures without a prior history, the drug may have breached the blood‑brain barrier and is now firing neurons out of sync.
Shortness of breath that appears out of nowhere can be a sign of pulmonary edema, especially with certain chemotherapeutic agents.
Weight gain and ankle swelling in just a few days can indicate that fluid is being retained due to hidden heart failure.
Even a subtle fever combined with joint pain may be the opening act of serum sickness, an immune complex reaction that can progress to glomerulonephritis.
A drop in blood pressure accompanied by dizziness is often the last gasp before shock sets in.
The key to survival is recognizing these symptoms within the first few hours and calling emergency services before the cascade becomes irreversible.
Keeping a meticulous log of the exact time each dose is taken and the onset of any new symptom can give physicians the timeline they need to pinpoint the offending agent.
Finally, never dismiss a mild rash or a fleeting headache; in the world of pharmacology, tiny clues often foreshadow catastrophic outcomes.
Jay Campbell
November 25, 2025 AT 01:37I appreciate the practical checklist; adding a reminder to discuss any over‑the‑counter supplements with the pharmacist can catch hidden interactions. Also, a quick pulse check after the first dose of a new medication might reveal tachycardia early. Simple habits like these can make a big difference without adding extra stress.
Laura Hibbard
December 4, 2025 AT 22:26Because nothing says ‘fun weekend’ like Googling “why am I turning purple” after a single dose.
Erin Leach
December 14, 2025 AT 19:15That feeling of panic when you see a rash spread is real, and it helps to have a trusted friend or family member who can drive you to the ER if you’re alone. Keeping a symptom diary on your phone makes it easier to share precise details with your doctor. Remember, you don’t have to face these scares solo.
Jennyfer Collin
December 24, 2025 AT 16:03One must consider that the prevailing narrative surrounding medication safety is largely curated by pharmaceutical conglomerates seeking to mitigate liability while preserving market dominance. The selective disclosure of adverse event statistics frequently omits data from proprietary clinical trials, thereby constructing a veneer of reassurance. Moreover, the integration of QR‑coded smart packaging, slated for 2026, may serve as a dual‑purpose surveillance mechanism, aggregating patient compliance data for corporate analytics rather than solely enhancing safety. Skepticism is warranted when industry‑driven initiatives are presented as altruistic public‑health solutions without independent oversight. Historically, similar “innovations” have been leveraged to reinforce patent extensions under the guise of patient benefit. Consequently, clinicians should remain vigilant and critically appraise the source of any safety alert before incorporating it into practice.
Nic Floyd
January 3, 2026 AT 12:52Pharmaco‑kinetics parametrics dictate dose‑interval optimization especially with CYP450 substrate polypharmacy it’s essential to model AUC peaks and troughs to avoid supratherapeutic exposure adherence monitoring can be facilitated by MEMS caps integration with EHR dashboards reduces ADE incidence by leveraging real‑time PK feedback loops.
Johnae Council
January 13, 2026 AT 11:11Honestly the whole “just read the label” spiel is a joke when half the warnings are in fine print that nobody actually reads. If you’re on a warfarin regimen and pop an NSAID you’re basically signing up for a bleed‑out. The article skips over how genetic polymorphisms can make even low‑dose opioids deadly. Bottom line: stay skeptical and demand a full interaction check before every refill.