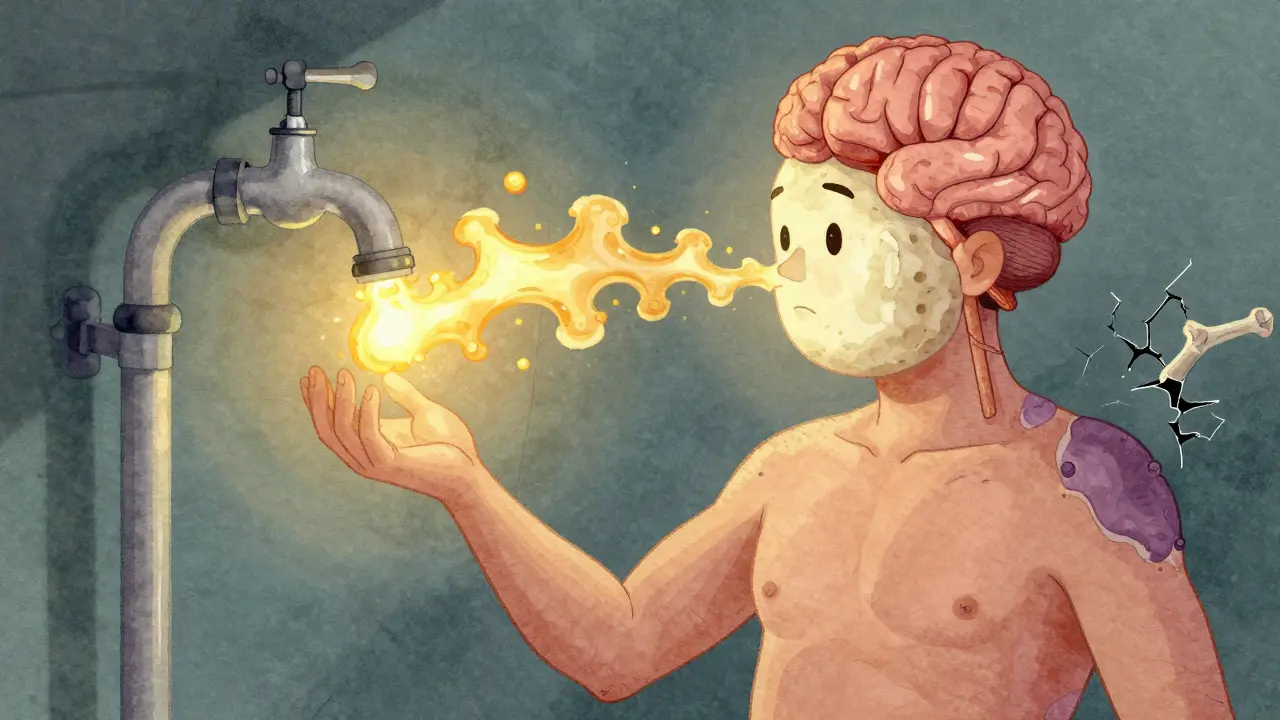
When your body makes too much cortisol, it doesn’t just cause weight gain or fatigue-it can break down your bones, wreck your heart, and turn your face into a moon-shaped balloon. This isn’t normal aging. It’s Cushing’s syndrome, a rare but serious hormonal disorder caused by prolonged exposure to high levels of cortisol. For most people, this isn’t about stress. It’s about a tumor in the pituitary or adrenal gland that’s secretly pumping out hormones like a broken faucet. And the best way to fix it? Surgery.
What Exactly Is Cushing’s Syndrome?
Cushing’s syndrome happens when your body is flooded with cortisol for months or years. Cortisol is your body’s natural stress hormone. It helps control blood sugar, blood pressure, and inflammation. But too much? It turns your body against itself. You gain weight in your belly and face while your arms and legs stay thin. Purple stretch marks appear on your skin. Your bones weaken. Your blood pressure spikes. You might feel exhausted all the time, even after sleeping. About 10 to 15 people out of every million get this each year. Most are women between 20 and 50. There are two main types: exogenous and endogenous. Exogenous Cushing’s comes from taking steroid pills-like prednisone-for asthma, arthritis, or autoimmune diseases. That’s the most common form, making up 80% of cases. But when the problem comes from inside your body? That’s endogenous Cushing’s. And that’s where surgery becomes critical.How Do Doctors Know You Have It?
Diagnosing Cushing’s isn’t simple. Symptoms overlap with obesity, depression, and aging. But three key tests confirm it:- Late-night saliva cortisol: Levels above 0.14 mcg/dL suggest excess cortisol.
- 24-hour urine cortisol: Over 50 mcg in a day is a red flag (normal is under 50).
- Low-dose dexamethasone test: If your cortisol doesn’t drop after taking a steroid pill, your body isn’t regulating itself properly.
Why Surgery Is the First Choice
Medication can lower cortisol, but it doesn’t fix the root cause. Drugs like pasireotide or mifepristone help manage symptoms, but they cost $5,000 to $10,000 a year and rarely cure the disease. Surgery, on the other hand, can remove the tumor and restore normal hormone levels-permanently. The Endocrine Society’s 2020 guidelines say surgery should be the first step for endogenous Cushing’s, if it’s safe and possible. Why? Because remission rates are far higher. For pituitary tumors (called Cushing’s disease), surgery removes the source. For adrenal tumors, removing the gland stops the cortisol flood.
Types of Surgery and Success Rates
There are three main surgical options, depending on where the tumor is:1. Transsphenoidal Pituitary Surgery
This is the most common procedure for Cushing’s disease. Surgeons go through the nose or upper lip to reach the pituitary gland-no scalp incisions. It takes 2 to 4 hours. Most patients leave the hospital in 2 to 5 days. Success depends on tumor size. For tumors under 10 mm (microadenomas), remission rates hit 80-90%. For larger tumors (macroadenomas), it drops to 50-60%. At high-volume centers-those doing over 20 pituitary surgeries a year-success climbs to 85-90%. At low-volume hospitals, it can be as low as 50%. Complications include cerebrospinal fluid leaks (2-5%), infection (1-3%), and temporary adrenal insufficiency (30-40% of patients). Permanent adrenal failure happens in 5-10% of cases.2. Laparoscopic Adrenalectomy
If the problem is a tumor on one adrenal gland (15-20% of endogenous cases), surgeons remove it using small incisions and a camera. This takes 1-2 hours. Hospital stay: 1-2 days. Success rate? 95%. Complications are rare-bleeding or infection happens in just 2-5% of cases. Recovery is faster than pituitary surgery. Most people feel better within weeks.3. Bilateral Adrenalectomy
This is a last-resort option. It’s done when both adrenal glands are overactive, or when pituitary surgery failed. Both glands are removed. Cortisol levels drop to zero-so you’re cured of Cushing’s. But now, you need lifelong hormone replacement: hydrocortisone and fludrocortisone. Without them, you’ll go into adrenal crisis. There’s a big risk: Nelson’s syndrome. In 40% of cases, the pituitary tumor grows back aggressively, causing dark skin, headaches, and vision problems. This is why doctors avoid this surgery unless absolutely necessary.What Happens After Surgery?
Surgery isn’t the end-it’s the start of a new routine. After removing the tumor, your body stops making cortisol. Your adrenal glands, which were “asleep” for years, need time to wake up. For most, that takes 3 to 6 months. During that time, you’ll take replacement steroids to avoid adrenal crisis. You’ll need frequent blood tests to adjust your dose. Too little? You’ll feel dizzy, nauseous, and weak. Too much? You’ll gain weight, get high blood pressure, and risk bone loss again. About 35% of patients still need steroid therapy a year after surgery. Some need it forever. You’ll also learn to give yourself “stress doses” during illness, injury, or surgery-because your body can’t make extra cortisol anymore. Recovery isn’t just physical. Many patients struggle with body image. Moon face and buffalo hump don’t vanish overnight. Weight loss takes months. Fatigue lingers. Depression is common. Support groups help. One patient on Reddit wrote, “I lost 40 pounds in 4 months after surgery. I cried the first time I saw my real face in the mirror.”Why Location Matters More Than You Think
Not all hospitals are equal. If you get surgery at a center that does fewer than 10 pituitary cases a year, your chance of remission drops to 50-60%. At top centers like Mayo Clinic, Barrow Neurological Institute, or OHSU, it’s 80-90%. Why? Experience. Surgeons who do this daily know how to spot hidden tumors. They use better tools-like 3D endoscopes and intraoperative cortisol monitors-that give real-time feedback during surgery. The FDA approved one such device in 2023, cutting confirmation time from 7 days to 24 hours. Insurance can be a hurdle. Medicare covers 85% of pituitary surgery costs. Private insurers deny 20% of adrenalectomy claims. If you’re denied, appeal. Many patients win after providing clinical guidelines from the Endocrine Society.
What If Surgery Doesn’t Work?
About 10-25% of patients relapse within 10 years. If cortisol rises again, options include:- Repeat pituitary surgery
- Radiation therapy (gamma knife or proton beam)
- Medical therapy with ketoconazole, mitotane, or cabergoline
- Adrenal-directed drugs like osilodrostat
What’s Next for Cushing’s Treatment?
New tech is making surgery better. A 2023 FDA-approved robotic scope gives surgeons 0.5mm resolution-so they can see tumors no one could find before. Clinical trials are testing 11C-metomidate PET/CT scans, which light up adrenal tumors with 95% accuracy. Robotic-assisted surgery is being tested to reduce surgeon fatigue during long cases. The NIH’s CUREnet registry is tracking over 1,000 patients. Early data shows: if you have surgery within 18 months of diagnosis, your remission rate is 85%. If you wait more than 2 years, it drops to 65%. The goal by 2030? Half of all Cushing’s surgeries done at specialized centers with multidisciplinary teams-endocrinologists, neurosurgeons, nurses, and mental health support. That’s the only way to bring mortality rates down to normal.Final Thoughts
Cushing’s syndrome isn’t just a hormonal glitch. It’s a slow, silent destruction of your body. Left untreated, it can kill you from heart attack, stroke, or infection. Surgery isn’t perfect-but it’s the only cure. The key is acting fast, finding the right surgeon, and sticking with follow-up care. If you’ve been told your symptoms are “just stress” or “you’re getting older,” push back. Get tested. If you have a tumor, don’t delay surgery. The longer cortisol runs wild, the harder it is to reverse the damage. Many patients say the same thing after surgery: “I didn’t know I was living in a fog until it lifted.”Can Cushing’s syndrome be cured without surgery?
Medication can control cortisol levels, but it rarely cures the disease. Drugs like pasireotide or mifepristone manage symptoms and are used when surgery isn’t possible. But they don’t remove the tumor, so cortisol levels often rise again. Long-term use is expensive and can cause liver damage, high blood sugar, or fatigue. Surgery remains the only way to eliminate the source of excess cortisol in endogenous cases.
How long does it take to recover after Cushing’s surgery?
Physical recovery varies. Most people leave the hospital in 1-5 days. But full recovery takes 3 to 6 months. Fatigue, mood swings, and muscle weakness linger as your body adjusts to normal cortisol levels. Weight loss happens gradually. Some patients return to work in 6 weeks; others need 4-6 months. Adrenal recovery can take up to a year, and some need lifelong hormone replacement.
Is Cushing’s surgery risky?
All surgery has risks. For transsphenoidal pituitary surgery, the main risks are cerebrospinal fluid leaks (2-5%), infection (1-3%), and temporary adrenal insufficiency (30-40%). Permanent hormone problems happen in 5-10%. For adrenal surgery, bleeding and infection are rare (2-5%). Bilateral adrenalectomy carries a 40% risk of Nelson’s syndrome. Success and safety depend heavily on surgeon experience-choose a high-volume center.
What happens if I don’t treat Cushing’s syndrome?
Untreated Cushing’s syndrome leads to severe complications: osteoporosis with fractures, uncontrolled diabetes, high blood pressure, heart disease, and increased risk of deadly infections. Studies show the 5-year mortality rate is 1.5 to 2 times higher than in healthy people. Even if symptoms seem manageable, the internal damage is ongoing. Early treatment saves lives.
Can Cushing’s come back after surgery?
Yes. Recurrence happens in 10-25% of patients within 10 years, especially with larger pituitary tumors or if not all tumor tissue was removed. Regular follow-up with cortisol tests and MRI scans is essential. If cortisol rises again, repeat surgery, radiation, or medical therapy may be needed. Early detection of recurrence improves outcomes.
Why do women get Cushing’s more often than men?
Women between 20 and 50 are 3 times more likely to develop Cushing’s, especially from pituitary tumors. The exact reason isn’t fully known, but hormones like estrogen may influence pituitary tumor growth. Adrenal tumors occur more evenly between genders but at an older age. The gender gap is strongest for Cushing’s disease, not adrenal causes.

Rajni Jain
December 26, 2025 AT 01:05i know someone who went through this and it was insane how fast she changed after surgery. her face went from moon-shaped to normal in like 3 months. she cried every time she looked in the mirror. i never realized how much cortisol messes with your soul, not just your body.
Natasha Sandra
December 26, 2025 AT 14:25OMG YES!! 🙌 I had a friend who was on prednisone for years and no one believed her until she got diagnosed. Like, ‘oh you’re just stressed’ - no, Karen, I’m not, I’m literally melting from the inside 😭 surgery saved her life. #CushingsAwareness
Erwin Asilom
December 27, 2025 AT 16:05The data on surgeon volume is critical. Centers performing fewer than 10 pituitary surgeries annually show significantly lower remission rates. This is not a procedure to be taken lightly or performed by inexperienced teams. The 2020 Endocrine Society guidelines are unequivocal: refer early to high-volume centers.
Sumler Luu
December 29, 2025 AT 06:09I work in endocrinology and see this too often. Patients get misdiagnosed for years because doctors think it’s just obesity or depression. The late-night saliva test is so simple - why isn’t it routine? If you have unexplained weight gain + fatigue + stretch marks, push for it. Don’t wait.
sakshi nagpal
December 31, 2025 AT 03:23It’s heartbreaking how many people suffer silently with this condition. In my country, access to specialized care is extremely limited. Many don’t even know what Cushing’s is. Education and early screening must be prioritized. This isn’t just a medical issue - it’s a human rights issue. We need global awareness and equitable access to diagnosis and surgery.
Sandeep Jain
January 1, 2026 AT 10:05my cousin had this and the doc said ‘take pills’ for 2 years before they finally did the mri. by then her bones were crumbling. why do docs wait so long? it’s not rocket science. if you look like a moon and feel like death, check your cortisol. i wish someone told us sooner.
roger dalomba
January 2, 2026 AT 05:33Oh great. Another ‘miracle cure’ post. Surgery? Really? You’re telling me we can’t just give people a better diet and some yoga? 😴
Amy Lesleighter (Wales)
January 2, 2026 AT 15:58after surgery my cortisol was zero for months. i had to carry hydrocortisone everywhere like a lifeline. no one tells you how lonely it is to be the only one who knows your body is broken. i lost 50 lbs. i got my laugh back. but i still wake up some days scared i’ll forget to take my pill. it’s not over when the bandages come off.
Becky Baker
January 4, 2026 AT 11:05Why are we letting foreign doctors do this? We have the best surgeons in the world here. If you’re not getting this done in the US, you’re doing it wrong.