Most people assume their prescriptions come straight from a factory in a standard pill, capsule, or liquid. But for thousands of patients, that’s not the case. Compounded medications are custom-made formulas crafted by pharmacists to fit individual needs that off-the-shelf drugs simply can’t meet. This isn’t science fiction-it’s everyday medicine for people with allergies, swallowing problems, or rare conditions. And while it solves real problems, it also carries hidden risks that many don’t know about.
Why Standard Pills Don’t Work for Everyone
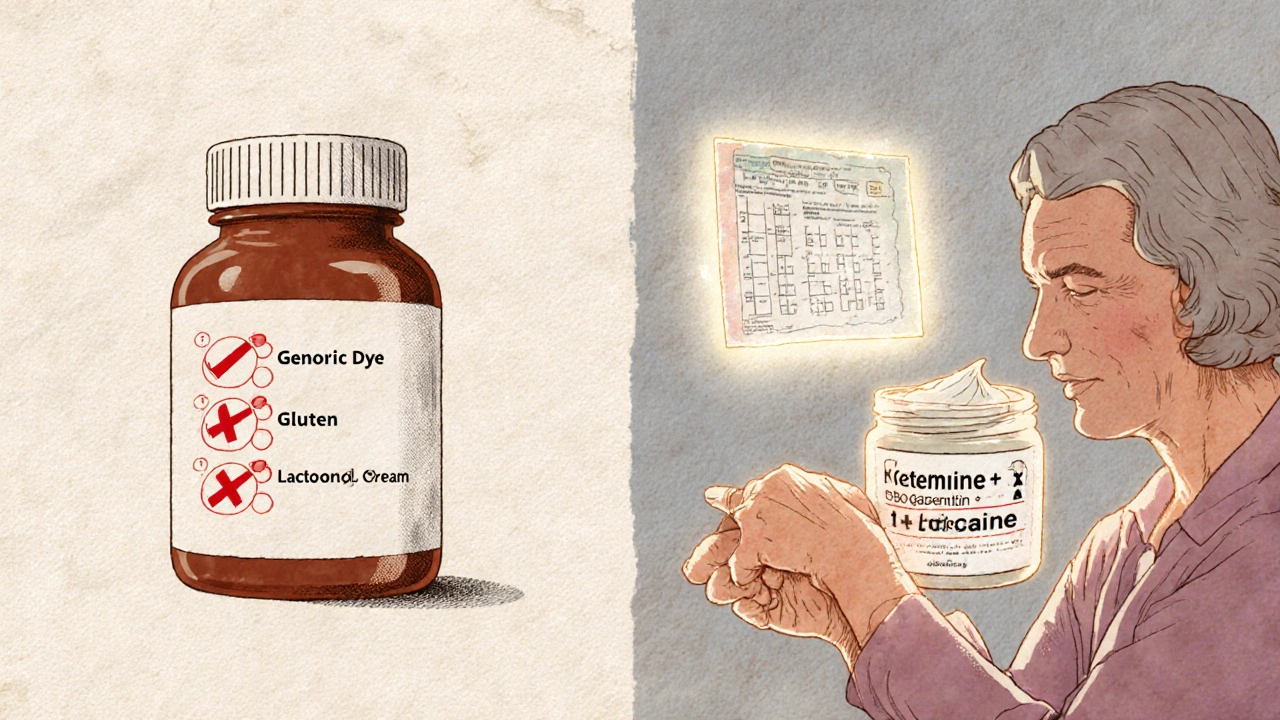
Imagine needing a dose of medication that doesn’t exist. Maybe you’re allergic to the dye in the pill. Or you’re a child who can’t swallow tablets. Or you’re an elderly person whose stomach can’t handle the fillers in commercial drugs. These aren’t rare edge cases. About 15 million Americans have documented allergies to common ingredients like lactose, gluten, or artificial coloring in medications. And up to 80% of kids struggle to swallow pills. For them, a standard prescription isn’t just inconvenient-it’s unusable. That’s where compounding comes in. Instead of forcing a patient to adapt to a drug, the pharmacist adapts the drug to the patient. A 1.5mg dose? If only 1mg and 2mg are sold, they can make it. A cream instead of a pill? Done. A flavorless liquid turned into cherry-flavored syrup? Easy. These aren’t just nice-to-haves. For many, they’re the only way to get treatment at all.How Compounded Medications Are Made
Compounding starts with a prescription from a doctor, nurse practitioner, or other licensed provider. It’s not something you can order online without one. The pharmacist then takes raw ingredients-active drugs and excipients like bases, binders, or flavorings-and mixes them under strict conditions. For non-sterile formulas (like creams or oral liquids), they work in clean rooms with controlled airflow. For sterile ones (like injections or IV bags), they use laminar flow hoods and follow even tighter protocols. The process can be simple: grinding a pill into powder and mixing it with a base for a topical gel. Or complex: combining three different hormones in precise ratios for bioidentical hormone therapy, or blending pain medications into a transdermal patch to avoid gut absorption issues. The key is precision. A small error in measuring can lead to too much or too little of the active ingredient-something that can have serious consequences.When Compounding Makes a Real Difference
There are three areas where compounded medications shine:- Pediatrics: Kids often refuse bitter-tasting medicines. A compounded cherry-flavored ADHD liquid can turn adherence from 40% to 95%, according to parent reports. That’s life-changing.
- Geriatrics: Older adults often take five or more pills a day. Combining them into one capsule or gel reduces confusion and improves compliance. It also helps those with digestion problems who can’t absorb pills properly-about 60-70% of elderly patients on multiple meds face this.
- Chronic pain and hormone therapy: Topical pain creams with multiple active ingredients (like ketamine, gabapentin, and lidocaine) deliver relief without the drowsiness or constipation of oral opioids. Bioidentical hormone creams allow for fine-tuned estrogen and progesterone levels that standard hormone pills can’t match.
The Hidden Risks: Safety Isn’t Guaranteed
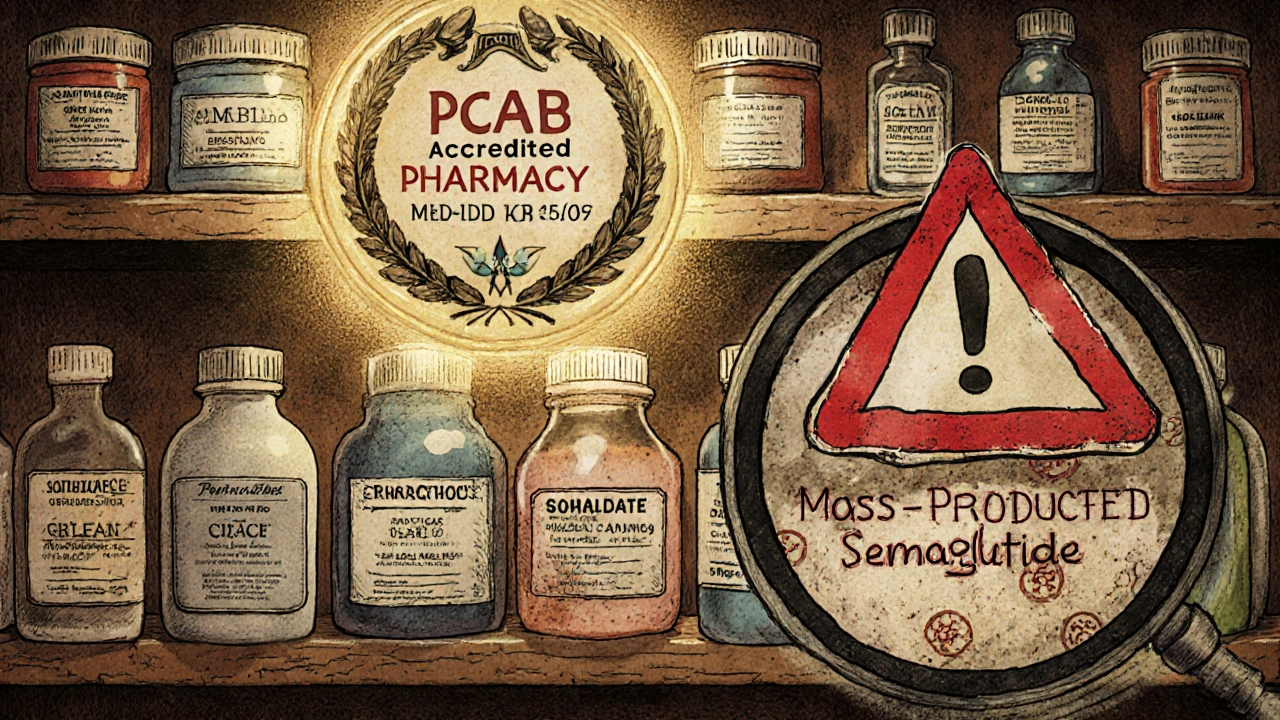
Here’s the catch: compounded medications are not FDA-approved. That means the agency doesn’t test them for safety, purity, or effectiveness before they’re given to patients. The FDA only steps in after something goes wrong. The 2012 meningitis outbreak tied to contaminated steroid injections from the New England Compounding Center killed 64 people and sickened nearly 800. It wasn’t a small pharmacy. It was a large-scale operation masquerading as a manufacturer. Since then, regulations tightened-but gaps remain. Between 2010 and 2020, compounded drugs accounted for just 1% of all prescriptions but 17% of all drug recalls. Why? Poor storage, incorrect labeling, contamination, or inconsistent dosing. One patient on PatientsLikeMe reported their compounded thyroid medication varied wildly in strength between batches-sending their TSH levels into chaos. That’s not an isolated case. And not all pharmacies are equal. Only about 350 of the 7,500 compounding pharmacies in the U.S. are accredited by the Pharmacy Compounding Accreditation Board (PCAB). That’s less than 5%. If you’re getting a compounded drug, ask: Is this pharmacy PCAB-certified? If not, why?Cost, Insurance, and Finding a Reliable Pharmacy
Compounded meds cost more. A basic non-sterile cream or liquid might run $30-$100, compared to $10-$50 for a generic pill. Sterile injections? Those can hit $200-$500 because they need special equipment, testing, and sterile environments. Insurance coverage is spotty. Medicare Part D covers only 42% of compounded claims. Private insurers vary widely. Some require prior authorization. Others won’t touch it unless it’s deemed medically necessary. Patients often pay out-of-pocket. To find a trustworthy pharmacy:- Look for PCAB accreditation. It’s the gold standard.
- Ask if they follow USP Chapter <795> for non-sterile compounding or <797> for sterile.
- Check if they test batches for potency and contamination-especially for hormones or pain creams.
- Don’t trust pharmacies that ship large volumes nationwide without a direct patient-provider relationship. That’s a red flag for illegal manufacturing.
The Big Picture: Exception, Not the Rule
Experts agree: compounded medications should be the exception, not the norm. If a commercial drug works, use it. The FDA, American Society of Health-System Pharmacists, and the American Pharmacists Association all stress this. Compounding fills gaps-but it shouldn’t replace the safety net of FDA-approved drugs. The rise of compounded weight loss drugs like semaglutide is a recent example of the line blurring. Some pharmacies are making large batches of these drugs, selling them like over-the-counter products. The FDA has issued multiple warning letters for this exact practice. These aren’t personalized treatments-they’re mass-produced imitations. The future of compounding lies in precision. Some pharmacies are now using genetic testing to tailor doses based on how a patient metabolizes drugs. For example, someone with a CYP2D6 gene variant might need half the standard dose of a painkiller. Compounding makes that possible. But without strict standards, this innovation could turn dangerous. The goal isn’t to replace regulated drugs. It’s to give patients who have nowhere else to turn a safe, effective option.What You Should Do
If you think you need a compounded medication:- Discuss it with your doctor first. Ask: Is there an FDA-approved alternative?
- Insist on a PCAB-accredited pharmacy. Don’t accept “we’ve always used this one.”
- Ask for a batch test report. Reputable pharmacies will provide it.
- Watch for side effects. If your symptoms change suddenly, or the medication looks or smells different, stop taking it and call your pharmacist.
- Keep a log. Note when you take it, how you feel, and any changes. This helps your provider spot inconsistencies.
Are compounded medications safe?
Compounded medications can be safe when made by accredited pharmacies following strict standards like USP <795> or <797>. But because they’re not FDA-approved, there’s no guarantee of purity or consistency. Always choose a PCAB-accredited pharmacy and ask for batch testing results.
Do I need a prescription for compounded medication?
Yes. Federal law requires a valid prescription from a licensed provider for any compounded medication. You cannot legally buy them over the counter or online without one. Any pharmacy offering compounded drugs without a prescription is operating illegally.
Why are compounded medications so expensive?
They cost more because they’re made in small batches by hand, using high-purity ingredients and specialized equipment. Sterile compounds require clean rooms, testing, and trained staff-all of which add to the price. A simple cream might cost $50, while an IV bag can run $500. Insurance often doesn’t cover them fully.
Can I get compounded versions of popular drugs like semaglutide?
Technically yes, but it’s risky. The FDA has cracked down on pharmacies compounding semaglutide and similar weight loss drugs in large quantities. These aren’t personalized-they’re copies of brand-name drugs made without FDA oversight. If you’re prescribed semaglutide, ask your doctor about the approved version instead.
How do I know if my compounded medication is working properly?
Track your symptoms and lab results. For example, if you’re on compounded thyroid medication, check your TSH levels regularly. If your blood pressure, pain levels, or energy change unexpectedly without reason, the dose may be inconsistent. Contact your pharmacist and ask for a batch test report. If they refuse, find a new pharmacy.


Deb McLachlin
November 17, 2025 AT 03:48Compounded medications represent a fascinating intersection of pharmacology and individualized care. The precision required to tailor dosages, eliminate allergens, or alter delivery methods speaks to the adaptability of modern pharmacy. Yet, the lack of standardized oversight is alarming. Without mandatory batch testing and transparent sourcing, we're essentially trusting individual pharmacists with lives, and that’s a responsibility that demands far more accountability than it currently receives.
Gordon Mcdonough
November 18, 2025 AT 21:13Why the hell are we letting some guy in a basement mix drugs without FDA checks?? We got national security threats from better things than this. These compounding places are just loopholes for quacks and crooks. I don't care if your kid won't swallow pills-use a liquid that's already approved! Stop letting pharmacists play god with my tax dollars and my family's health
Sridhar Suvarna
November 19, 2025 AT 14:13Compounding is not a luxury-it is a necessity for many who live at the margins of conventional medicine. In India, we see this daily: children with rare metabolic disorders receiving custom formulations because no commercial product exists. The challenge lies not in the practice itself but in the absence of global standards. We must elevate accreditation, not demonize innovation. A regulated system, not a banned one, is the path forward.
Joseph Peel
November 21, 2025 AT 04:53The structural integrity of pharmaceutical regulation must not be compromised under the guise of personalization. While the intent behind compounding is commendable, the execution-particularly when unaccredited-is a public health liability. The 2012 outbreak was not an anomaly; it was an inevitability born of deregulation. We must enforce USP standards universally and require full traceability for every compounded product.
Kelsey Robertson
November 21, 2025 AT 11:19Oh, so now we're romanticizing backyard pharmacies because some kid doesn't like bitter medicine? Let me guess-next you'll say we should let people brew their own chemo in their garage because 'it's personalized.' The FDA exists for a reason. If you can't swallow a pill, use a patch. If you're allergic to dye, use a different brand. Stop pretending that compounding is some noble art-it's just a loophole for people who don't want to follow the rules.
Bill Machi
November 22, 2025 AT 02:39Let’s be real. Most of these compounding pharmacies are just profit-driven operations hiding behind ‘customization.’ They charge ten times the price of a generic and then act like they’re saints. And don’t get me started on the hormone creams-half of them are just glorified lotions with a fancy label. The FDA should shut down 90% of these places and force everyone to use approved drugs. End of story.
Elia DOnald Maluleke
November 23, 2025 AT 16:24In the grand tapestry of human healing, compounding is the artisan’s brushstroke-delicate, necessary, and often invisible. Yet, when the brush is dipped in untested pigments, the entire canvas risks decay. The tragedy is not in the act of creation, but in the absence of guardianship. We must not abandon the artisan, but demand that the studio be sanctified by science, not by convenience.
satya pradeep
November 25, 2025 AT 11:11My cousin in Mumbai got a compounded pain cream after her chemo left her skin raw-standard meds burned like fire. This stuff? Saved her nights. But yeah, the pharmacy she used? No PCAB, no testing. She just trusted the guy who had a 10-year history in the neighborhood. Sometimes, in places with no other options, trust is all you got. We need better systems, not just more red tape.
Prem Hungry
November 25, 2025 AT 12:55For those struggling with swallowing pills or managing multiple meds, compounding is a lifeline. I’ve seen elderly patients regain independence because their meds were combined into one gel. The cost is high, yes-but the cost of non-compliance is higher. Let’s focus on expanding access to accredited labs, not shutting down hope. Innovation should be encouraged, not feared.
Leslie Douglas-Churchwell
November 25, 2025 AT 17:10Big Pharma hates compounding because it threatens their monopoly. The FDA? Complicit. The 2012 outbreak? Staged to scare people into accepting their overpriced, mass-produced junk. Those ‘custom’ hormone creams? They’re using the same base as your Walmart lotion-just with a fancy label and a $300 markup. And don’t get me started on how they’re hiding behind ‘prescription’ loopholes. Wake up-this is corporate control disguised as care. 🚩🧪💊
shubham seth
November 26, 2025 AT 22:05Let’s be honest-compounding is the Wild West of pharmacy. Some folks are angels with beakers, others are snake oil salesmen in lab coats. The fact that less than 5% are PCAB-certified? That’s not a feature, it’s a fucking crime. And don’t even get me started on the ‘bioidentical hormone’ cult-half of them are just repackaged estrogen with a yoga retreat vibe. This ain’t medicine, it’s a cult with a pharmacy license.
Kathryn Ware
November 28, 2025 AT 19:47I’ve been a pharmacist for 22 years, and I’ve seen firsthand how compounding changes lives. A 92-year-old woman with severe GERD couldn’t swallow anything-so we made her a transdermal patch for her blood pressure med. She started sleeping again, eating, laughing. But I also know the risks. I only work with PCAB-certified labs. I test every batch. I document everything. It’s a ton of work-but when you’re holding someone’s life in your hands, cutting corners isn’t an option. We need more pharmacists like this, not fewer. And yes, insurance should cover this-it’s not a luxury, it’s essential care.
kora ortiz
November 30, 2025 AT 12:22Compounding isn’t about rebellion-it’s about resilience. When the system fails, we adapt. I’ve seen toddlers thrive on flavorless, dye-free meds. I’ve seen veterans with chronic pain finally sleep without opioids. This isn’t fringe medicine-it’s human medicine. The solution isn’t to ban it, but to fund better oversight, train more compounding specialists, and demand transparency. Let’s elevate the standard, not eliminate the option.
Jeremy Hernandez
December 1, 2025 AT 06:14Yeah sure, ‘personalized medicine’-until your grandma’s ‘custom’ thyroid med turns out to be half the dose one month and double the next. Then she’s in the ER with a heart attack. These places are barely regulated. The FDA doesn’t even know half of them. And don’t tell me about ‘trust your pharmacist’-most of them are just following orders from a guy who bought a pharmacy license off eBay. This is a disaster waiting to happen again.
Tarryne Rolle
December 1, 2025 AT 14:26It’s ironic that we celebrate ‘personalized care’ while ignoring the fact that true personalization requires systemic equity. If you’re poor, you can’t afford a PCAB-certified pharmacy. If you’re rural, you can’t access one at all. So we’re not expanding care-we’re creating a two-tiered system where the privileged get safe, custom meds and everyone else gets toxic generics or nothing. That’s not innovation. That’s inequality with a white coat.