Chronic eczema isn’t just dry, itchy skin. It’s a broken skin barrier that won’t heal on its own. If you’ve been using lotions that don’t seem to help, or if your skin flares every time you touch soap, laundry detergent, or even sweat-you’re not alone. About 1 in 3 children and 1 in 50 adults live with this condition, and the numbers keep rising. What most people don’t realize is that the root cause isn’t allergies or stress-it’s a physical breakdown in the skin’s outer layer. Fix that, and the itching, redness, and flares start to fade.
Why Your Skin Barrier Is the Key
Your skin isn’t just a surface. It’s a layered defense system. The top layer, called the stratum corneum, is made of dead skin cells held together by lipids-fats like ceramides, cholesterol, and free fatty acids. Think of it like a brick wall. The bricks are skin cells, and the mortar is these lipids. In chronic eczema, the mortar is missing. Studies show people with this condition have 30-50% less ceramide, especially one type called ceramide 1, which is critical for holding everything together. That’s why water escapes (called transepidermal water loss, or TEWL), and irritants, bacteria, and allergens slip in.
This isn’t a side effect of inflammation-it’s the cause. A 2023 study from the American Academy of Dermatology found that in babies at high risk for eczema, the barrier breaks down 3 to 6 months before the first rash appears. That means if you can repair the barrier early, you can stop eczema before it starts. For adults, it’s never too late. Consistent barrier repair reduces flare frequency by 40-60% over time, according to long-term studies in the Journal of Investigative Dermatology.
What Actually Repairs the Barrier
Not all moisturizers are created equal. Basic petroleum jelly or glycerin creams might feel soothing, but they don’t fix the problem. They’re like putting tape over a hole in a pipe-it masks the leak but doesn’t seal it. True barrier repair requires replacing the missing lipids in the exact ratio your skin needs: ceramide:cholesterol:free fatty acids at 1:1:1.
Clinical trials show products with this ratio restore barrier function in 87% of users, compared to just 52% with regular emollients. These aren’t just fancy marketing terms. Look for products that list specific ceramide types (ceramide NP, AP, EOP), cholesterol, and free fatty acids like linoleic acid on the ingredient list. Brands like CeraVe, EpiCeram, and Atopiclair use this formula. One user on Reddit tracked their TEWL (a lab measurement of skin barrier strength) dropping from 38 to 15 g/m²/h after 30 days of using CeraVe-meaning their skin went from leaking like a sieve to holding moisture like a sealed container.
Even the pH matters. Your skin’s natural pH is slightly acidic-around 4.5 to 5.5. If a product is too alkaline (like regular soap, which is pH 9-10), it shuts down enzymes that make ceramides. Products with pH 5.0-5.5 keep those enzymes working at 90% efficiency. That’s why some barrier creams sting at first-they’re acidic. It’s not a reaction; it’s your skin adjusting.
Common Triggers You Can’t Ignore
Once the barrier is broken, even small things can set off a flare. The big ones are:
- Harsh soaps and detergents - Sodium lauryl sulfate (SLS) and fragrances strip lipids. Switch to fragrance-free, soap-free cleansers like Cetaphil Gentle Skin Cleanser.
- Heat and sweat - When you sweat, salt and ammonia sit on the skin and irritate the damaged barrier. Shower immediately after exercise and pat dry-not rub.
- Dry air - Indoor heating and air conditioning drop humidity below 30%. Use a humidifier in your bedroom. It’s not optional if you live in a dry climate.
- Staphylococcus aureus - This bacteria thrives on broken skin. In fact, 90% of eczema lesions have it. Barrier repair cuts colonization by 65-75%, but if you’re still flaring, your doctor may recommend a bleach bath (½ cup bleach in a full tub, soak 10 minutes twice a week) to reduce bacterial load.
- Stress and sleep deprivation - Not direct causes, but they raise inflammation hormones that worsen itching. It’s a cycle: itch → scratch → sleepless → stressed → itch more.
Keep a simple log: what you ate, touched, or did 24 hours before a flare. Most people find 2-3 consistent triggers. Eliminate those first.

How to Actually Stop the Itch
Itch isn’t just annoying-it’s damaging. Scratching breaks the barrier even more, creating a vicious loop. Here’s how to break it:
- Cool compresses - Soak a clean cloth in cold water, wring it out, and press it on the itchy area for 5-10 minutes. This cools nerve endings and interrupts the itch signal.
- Topical menthol or pramoxine - These ingredients temporarily block itch nerves. Look for OTC creams with 1% menthol or 1% pramoxine. Avoid numbing agents like lidocaine long-term-they can irritate.
- Wet wrap therapy - After applying moisturizer, cover the area with damp cotton clothing or gauze, then top with dry layers. This traps moisture and reduces scratching during sleep. Studies show it cuts nighttime scratching by 70%.
- Antihistamines at night - While they don’t stop the root cause, sedating ones like hydroxyzine or diphenhydramine help you sleep through the itch. Use them short-term, not daily.
Don’t rely on steroids alone. Topical steroids like betamethasone reduce inflammation fast, but they thin the skin over time. That’s why barrier repair is the foundation-it lets you use less steroid. One 7-year-old case study showed barrier repair alone reduced steroid use by 80% over 6 months.
How to Apply Barrier Creams Right
Applying moisturizer the wrong way wastes time and money. Here’s what works:
- Apply within 3 minutes after bathing. Water trapped in the skin locks in moisture better than any cream.
- Use the fingertip unit method: one unit (the amount squeezed from a tube onto your index finger from tip to first crease) covers two adult hands. For arms or legs, use 2-3 units per limb.
- Apply twice daily-morning and night. Even on good days.
- Wait 15 minutes after moisturizing before applying steroid creams. Mixing them reduces effectiveness.
- Don’t rub. Pat or press gently. Rubbing damages the fragile barrier.
Most people see results in 2-4 weeks. But you need 92% consistency to get full benefit, according to NIH data. That means missing one day every two weeks is okay-but missing two days in a row? That’s when flares creep back.
When Barrier Repair Isn’t Enough
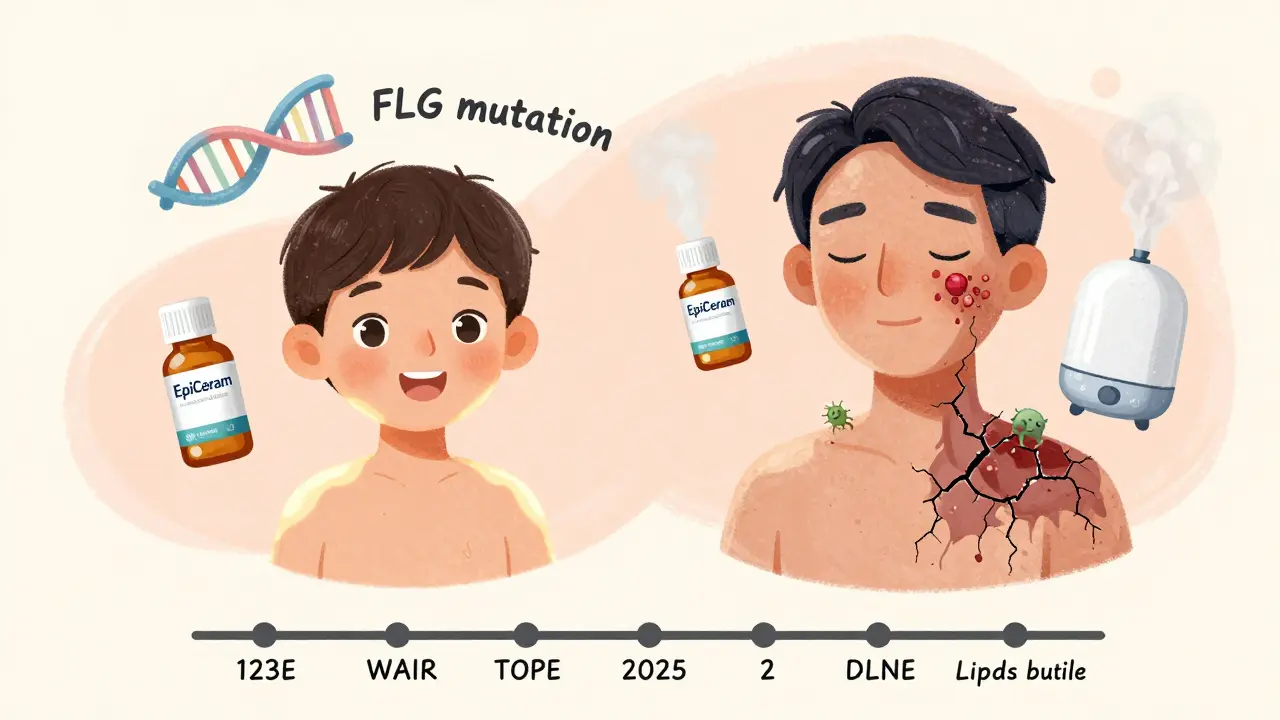
Here’s the hard truth: 30-40% of people with severe eczema have a genetic mutation in the filaggrin gene (FLG). This mutation affects half of all moderate-to-severe cases. It means your body literally can’t make enough of the protein that holds skin cells together. No amount of ceramide cream will fix that.
If you’ve tried barrier repair for 12 weeks with no improvement, talk to a dermatologist. You may need a JAK inhibitor (like upadacitinib) or a biologic (like dupilumab). These drugs target the immune system’s overreaction, which becomes self-sustaining when the barrier stays broken too long. The good news? Combining barrier repair with these treatments works better than either alone. One 2023 NEJM study showed patients on both had 60% fewer flares than those on medication alone.
And if cost is an issue? Barrier repair creams cost 2-3 times more than basic lotions-$28.50 for 200g versus $9.99. But Medicare and some private insurers cover prescription versions like EpiCeram. Ask your doctor for a prescription even if you’re buying OTC-it can cut your out-of-pocket cost by 50% or more.
What’s Next for Eczema Treatment
The future is personalized. Companies like 23andMe are partnering with dermatology labs to match barrier repair products to your filaggrin mutation status. Early algorithms are 85% accurate at predicting which ceramide blend will work for you. In 5 years, your eczema treatment might be based on a DNA test.
Other emerging options include platelet-rich plasma (PRP) therapy, which uses your own blood to stimulate skin repair, and microbiome-targeted creams that reintroduce good bacteria like Staphylococcus hominis to outcompete the bad ones. The International Eczema Council predicts barrier repair will become half of all eczema treatment by 2030.
But right now, the best tool you have is simple: repair the barrier, avoid triggers, control the itch. Do it consistently, and you’re not just managing eczema-you’re reclaiming your skin.
Can I use regular lotion for chronic eczema?
Regular lotions with water, glycerin, or petrolatum may feel soothing but don’t repair the skin barrier. They’re like putting a bandage on a broken pipe-they mask the leak but don’t fix it. For chronic eczema, you need products with specific lipids: ceramides, cholesterol, and free fatty acids in a 1:1:1 ratio. These are found in barrier repair creams like CeraVe, EpiCeram, or Atopiclair.
Why does my eczema cream sting when I apply it?
Stinging is common with barrier repair creams because they’re formulated at a slightly acidic pH (5.0-5.5) to activate enzymes that rebuild ceramides. Healthy skin doesn’t sting, but damaged skin with open cracks or inflammation reacts. It usually fades after 3-7 days of daily use. If it persists or worsens, switch to a gentler formula or consult a dermatologist.
How long until I see results from barrier repair?
Most people notice less dryness and fewer flares in 2-3 weeks. But full barrier restoration takes 4-6 weeks of twice-daily use. Clinical studies show TEWL (water loss) drops by 30-50% after 2 weeks and continues improving up to 12 weeks. Consistency matters more than product price-missing even one application every few days slows progress significantly.
Is eczema caused by allergies?
Allergies can worsen eczema, but they’re not the root cause. The primary problem is a genetic and physical breakdown in the skin barrier. Once that’s broken, allergens like dust mites or pollen can penetrate deeper and trigger inflammation. That’s why barrier repair often reduces allergic reactions-even without avoiding triggers. Think of it like fixing a leaky roof: once it’s sealed, rain doesn’t get in, no matter how hard it pours.
Should I stop using steroids if I start barrier repair?
No-don’t stop steroids abruptly. Barrier repair lets you use them less over time. Use both: apply your barrier cream first, wait 15 minutes, then apply steroid only to active flares. As your skin heals, your doctor can help you reduce steroid frequency. Many patients eventually stop steroids entirely once the barrier is strong enough to prevent flares.
Are expensive barrier creams worth it?
Yes-if they contain the right ingredients. A $30 cream with 3% ceramides, 2% cholesterol, and 1% fatty acids will outperform a $10 cream with just petrolatum and glycerin. But you don’t need the priciest brand. Generic versions from pharmacies (like CeraVe’s store-brand alternatives) often match the formula. Check the ingredient list, not the price tag. Also, ask your doctor about insurance coverage-some prescription barrier creams are covered at 80%.
Can children use barrier repair creams?
Yes, and they benefit even more. A 2023 study showed infants with early barrier repair had 70% fewer eczema flares by age 2. Use fragrance-free, pediatric-tested formulas. Apply immediately after bath, twice daily. For babies, even 2 grams (a pea-sized amount) per limb is enough. Consistency is key-start early, and you may prevent chronic eczema from developing.


THANGAVEL PARASAKTHI
February 8, 2026 AT 20:00Frank Baumann
February 9, 2026 AT 02:00Scott Conner
February 10, 2026 AT 15:16Alex Ogle
February 11, 2026 AT 17:34Brandon Osborne
February 13, 2026 AT 15:55MANI V
February 14, 2026 AT 13:56Susan Kwan
February 16, 2026 AT 02:40Random Guy
February 17, 2026 AT 12:16Ryan Vargas
February 18, 2026 AT 12:09Jessica Klaar
February 20, 2026 AT 06:48PAUL MCQUEEN
February 20, 2026 AT 21:41Angie Datuin
February 21, 2026 AT 21:19Camille Hall
February 23, 2026 AT 11:42Ritteka Goyal
February 23, 2026 AT 18:33Ashlyn Ellison
February 23, 2026 AT 19:05