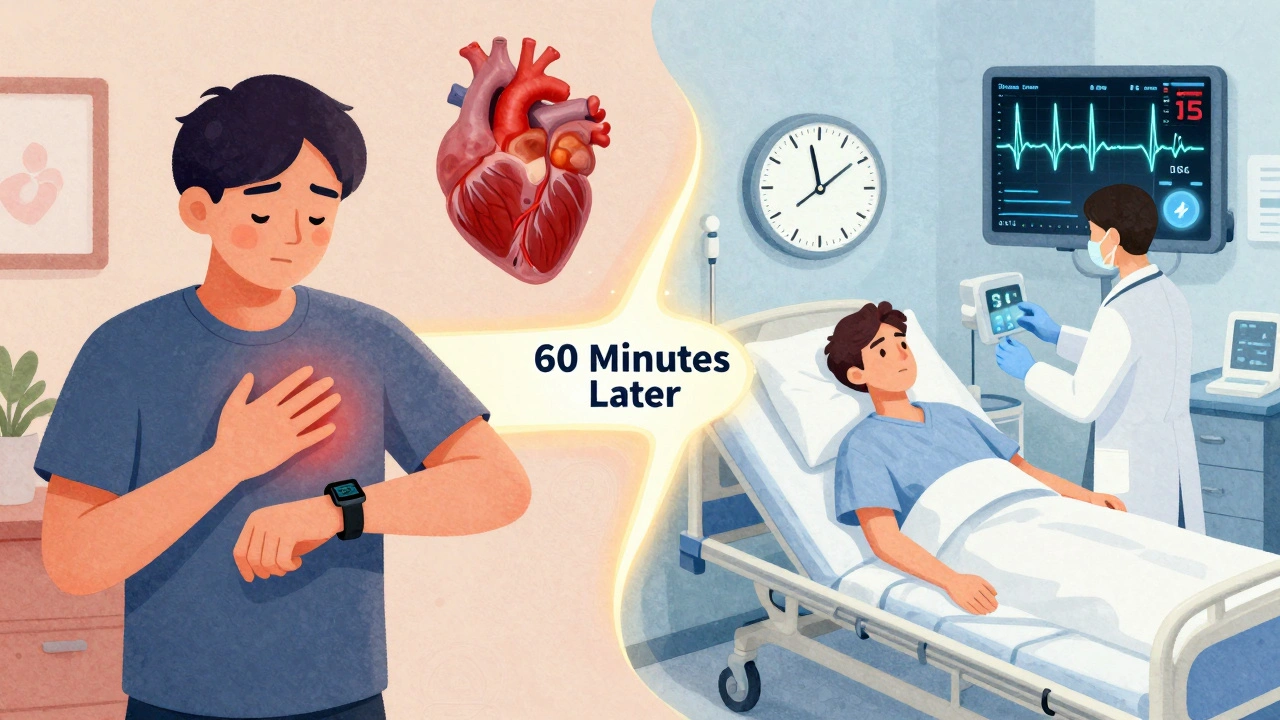
When your chest hurts, your brain screams: heart attack. But not every chest pain is a heart attack. And not every heart attack looks like the movies show. The real danger isn’t the pain itself-it’s waiting too long to act when you should’ve gone straight to the emergency department.
What Chest Pain Really Means
Chest pain isn’t just a sharp stab or crushing weight in the middle of your chest. It can feel like pressure, tightness, burning, or even just a strange fullness. And it doesn’t even have to be in your chest. You might feel it in your jaw, down your left arm, in your back, or deep in your upper belly. Some people-especially women, older adults, and those with diabetes-don’t feel chest pain at all. Instead, they get sudden fatigue, nausea, dizziness, or shortness of breath with no obvious cause.This isn’t guesswork. The 2021 American Heart Association and American College of Cardiology guidelines define chest pain as any discomfort in the chest, shoulders, arms, neck, jaw, or upper abdomen, especially when paired with sweating, nausea, or unexplained tiredness. These are called anginal equivalents-signs your heart is struggling, even if it doesn’t scream.
When to Call 9-1-1, Not Drive Yourself
If you’re experiencing chest discomfort that lasts more than a few minutes-or comes and goes over 15-20 minutes-don’t wait. Don’t text a friend. Don’t Google it. Don’t hope it’ll pass. Call emergency services right away.Why? Because every minute counts. If your heart muscle is being starved of oxygen, the clock is ticking. Studies show that people who drive themselves to the hospital have a 25-30% higher risk of complications than those transported by EMS. Emergency crews can start monitoring your heart, give you aspirin, and even transmit your ECG to the hospital before you arrive. That’s a 20-30 minute head start on treatment.
Here’s the short list of red flags that mean you need an ambulance now:
- Chest pain or pressure lasting more than 5 minutes
- Pain that spreads to your arm, jaw, neck, or back
- Sudden sweating, especially cold, clammy sweat
- Nausea, vomiting, or sudden dizziness
- Shortness of breath without exertion
- Heart rate over 100 bpm or breathing faster than 20 times per minute
- Low blood pressure (below 90 mmHg)
- Feeling like you’re going to pass out
If you have even one of these, don’t debate it. Call 9-1-1. The hospital can send a team ready to act the moment you walk in.
What Happens When You Arrive at the ED
When you get to the emergency department, the first thing they do is check if you’re sick or not sick. It’s not about how you feel-it’s about what your body is telling them. Is your skin pale? Are you sweating? Is your heart racing? Are you struggling to breathe? That’s the clinical gestalt-your doctor’s gut feeling based on your appearance and vital signs.Then, within 10 minutes of arrival, you’ll get a 12-lead ECG. No delays. No excuses. This test is the fastest, cheapest, and most powerful tool to spot a heart attack. It can show if you’re having a STEMI-the most dangerous kind-where a major artery is completely blocked. If it’s there, the hospital’s cath lab team springs into action. The goal? Get you to the catheterization table in under 90 minutes.
After the ECG, they’ll take a blood sample for a high-sensitivity troponin test. Troponin is a protein released when heart muscle is damaged. The new generation of tests can detect tiny changes within an hour. In fact, 70-80% of chest pain patients can be ruled out for a heart attack within 1-2 hours using this method.
They’ll also check your blood pressure, oxygen levels, and heart rhythm. If you have signs of heart failure-like crackles in your lungs or a third heart sound (S3 gallop)-they’ll act fast. If you’re stable, they might use the HEART score: a simple tool that looks at your history, ECG, age, risk factors, and troponin level to decide if you’re low, medium, or high risk.

When You Don’t Need the ED
Not every chest discomfort is an emergency. If you’ve had similar pain before, it’s been diagnosed as stable angina, and it goes away with rest or nitroglycerin, you’re likely okay to call your doctor the next day. But only if:- The pain is predictable-happens with exertion, goes away with rest
- You’ve been diagnosed by a cardiologist before
- You have your prescribed medication on hand
- No new symptoms like sweating, nausea, or trouble breathing
If any of those conditions aren’t met, don’t risk it. Play it safe. Go to the ED.
Also, some chest pain has nothing to do with your heart. Acid reflux, muscle strain, panic attacks, lung infections, or even shingles can mimic cardiac pain. But here’s the catch: you can’t tell the difference alone. That’s why the ED exists-to rule out the life-threatening stuff fast.
What You’ll Be Told After Testing
If your ECG and troponin are normal and you’re low-risk, you might be sent home with follow-up instructions. That doesn’t mean you’re off the hook. About 5-10% of people who leave the ED with a "normal" workup later have a heart attack within 30 days. That’s why follow-up is non-negotiable.You’ll likely be referred to a cardiologist for stress testing, a coronary CT angiogram (CCTA), or other imaging. CCTA is more accurate than a treadmill test for spotting blocked arteries, especially if you’re under 65 and have no prior heart disease. But if you have kidney problems or an allergy to contrast dye, stress testing is still the go-to.
Some patients are diagnosed with INOCA-Ischemia with Non-Obstructive Coronary Arteries. That means their heart isn’t getting enough blood, but their arteries aren’t clogged. It’s real, it’s serious, and it’s often missed. If you’ve had chest pain, normal angiograms, but still feel unwell, keep pushing for answers.
What’s Changing in 2025
By 2025, most U.S. hospitals will use AI to help read ECGs. These systems can spot subtle changes humans miss-like tiny ST-segment shifts or early T-wave inversions that signal a heart attack hours before it fully develops. Early tests show 98.5% accuracy. That means faster diagnosis, fewer missed cases, and better outcomes.High-sensitivity troponin is now used in 90% of U.S. emergency departments. That’s a huge shift from just five years ago. It’s why you can now be ruled out for a heart attack in under two hours instead of waiting six to eight.
But the biggest change isn’t technology. It’s mindset. The guidelines now stress shared decision-making. Your doctor should explain your risk, the pros and cons of testing, radiation exposure from scans, and costs-not just tell you what to do. You have a right to understand why you’re being sent for a test or held overnight.
What to Do Next
If you’ve ever had chest pain-even once-talk to your doctor. Ask: "Could this have been a heart issue?" Get your risk factors checked: blood pressure, cholesterol, blood sugar, and family history. If you’re over 40, smoke, have diabetes, or have a family history of early heart disease, get a baseline ECG and lipid panel.Keep aspirin (81 mg) in your medicine cabinet. If you ever suspect a heart attack, chew one tablet while waiting for EMS. It’s not a cure, but it can reduce damage.
And remember: if you’re unsure, go. Better to be safe than sorry. Every year, 6 to 8 million people go to the ED with chest pain. Only 1 in 10 has a heart attack. But if you’re that one person? Waiting could cost you your life.
Is chest pain always a sign of a heart attack?
No. Chest pain can come from many causes like acid reflux, muscle strain, anxiety, lung issues, or even shingles. But because heart attacks can mimic these conditions, it’s dangerous to assume it’s "just gas" or "indigestion." Always get checked if the pain is new, unexplained, or lasts more than a few minutes.
Can I wait to see my doctor instead of going to the ER?
Only if your symptoms are stable, predictable, and you’ve been diagnosed before with stable angina. If the pain is new, worsening, happening at rest, or comes with sweating, nausea, or shortness of breath-go to the ER. Delaying care can lead to permanent heart damage or death.
What if I’m not sure if it’s serious?
If you’re unsure, call emergency services. Paramedics are trained to assess chest pain on the spot and can start life-saving treatment before you even reach the hospital. It’s better to have them come for nothing than to wait and regret it later.
Do women experience chest pain differently than men?
Yes. While men often report classic crushing chest pain, women are more likely to have symptoms like extreme fatigue, nausea, jaw or back pain, dizziness, or shortness of breath without chest pressure. These "atypical" symptoms are often dismissed, leading to delayed diagnosis. Don’t assume you’re fine just because you don’t have "typical" chest pain.
What’s the HEART score, and why does it matter?
The HEART score is a tool doctors use to quickly assess your risk of heart attack based on five factors: your History of chest pain, ECG results, Age, Risk factors (like smoking or diabetes), and Troponin levels. A score of 0-3 means low risk, 4-6 is intermediate, and 7-10 is high risk. It helps decide whether you can go home or need to be admitted-making care faster and safer.
Can I rely on home ECG devices like Apple Watch?
Home ECG devices can detect irregular heart rhythms like atrial fibrillation, but they can’t reliably rule out a heart attack. They miss subtle changes that hospital-grade ECGs catch. Don’t use them to avoid the ER. If you have chest pain, go to the hospital-even if your watch says "normal."
What happens if I go to the ER and it’s not a heart attack?
You’ll still get a full evaluation to find the real cause-whether it’s acid reflux, lung issues, muscle strain, or anxiety. Even if it’s not cardiac, your symptoms matter. The ER’s job is to rule out life-threatening causes first. You’re not wasting anyone’s time-you’re doing the right thing.
How soon should I follow up after being discharged?
If you were discharged after chest pain evaluation, you should see a cardiologist or your primary doctor within 1 to 7 days. Even if tests were normal, 5-10% of people have a heart event within 30 days. Follow-up testing like stress tests or CCTA may be needed to catch hidden problems.


Emily Haworth
December 12, 2025 AT 13:34Okay but have you seen the news about how the EDs are secretly using AI to flag people who "don’t look sick enough"? 😳 I swear my cousin went in with chest pain and they told her "it’s probably anxiety"... then she collapsed at home 3 hours later. They’re prioritizing cost over lives. 🚨 #EDConspiracy
Webster Bull
December 13, 2025 AT 16:54Just chew an aspirin and call 911. No debates. No Googling. No waiting. Your heart doesn’t care if you’re "not sure." It just needs you to move. 🏃♂️💨
Emma Sbarge
December 14, 2025 AT 13:01This is why America needs better healthcare access. If you can’t afford to go to the ED, you’re already at a disadvantage. And don’t get me started on how insurance companies deny ambulance rides. We’re letting people die over paperwork.
Sheldon Bird
December 14, 2025 AT 21:01You’re not being dramatic if your chest hurts. You’re being smart. And if someone tells you to "just relax," they’ve never held someone’s hand while they’re having a heart attack. I’ve been there. Go. Now. 🙏
Karen Mccullouch
December 15, 2025 AT 15:33They don’t want you to know this, but the real reason they push ECGs and troponin tests is so they can bill you for $12,000. I work in billing. They don’t care if you live or die-they care if the code gets approved. 💸
Michael Gardner
December 17, 2025 AT 08:10Wait, so if I have acid reflux and it feels like a heart attack, I should still go? But what if I go every time I have heartburn? Isn’t that just clogging up the system? 🤔
Jennifer Taylor
December 18, 2025 AT 19:33MY BEST FRIEND DIED BECAUSE SHE WAITED. She said "it’s probably just stress"... then she woke up in the morgue. Don’t be her. Don’t be that person who texts their friend instead of calling 911. I’m not joking. I’m not dramatic. I’m just angry. 🖤
Hamza Laassili
December 20, 2025 AT 01:23So… if you’re under 40, skinny, and don’t smoke… you’re fine right? WRONG. My nephew was 28, ran marathons, and had a heart attack from a genetic condition. No warning. No risk factors. Just… dead. Don’t assume you’re immune.
Constantine Vigderman
December 21, 2025 AT 08:17Guys, I used to ignore chest pain like it was nothing… then I had a mini-heart-attack at the gym. They saved me because I called 911. Now I carry aspirin in my pocket, my car, my gym bag. I’m alive because I didn’t overthink it. You can be too. 💪❤️
Casey Mellish
December 22, 2025 AT 09:03Here in Australia, we’ve got a similar system-but the ambulance service is free and dispatched within 8 minutes. No billing drama. No waiting. Just help. Maybe we should stop treating healthcare like a subscription service and start treating it like a human right.
Tyrone Marshall
December 23, 2025 AT 06:11One of the most powerful things you can do is educate your family. My mom thought chest pain meant "you’re just stressed." I sat her down, showed her the guidelines, and now she calls 911 at the first sign. That’s how lives are saved-not by technology, but by conversation.
Tom Zerkoff
December 23, 2025 AT 15:38It is imperative to underscore that the HEART score, while statistically robust, is not infallible. Clinical judgment remains the cornerstone of triage, and overreliance on algorithmic tools may inadvertently obscure nuanced presentations, particularly in patients with atypical symptomatology.
Yatendra S
December 23, 2025 AT 19:46Life is a cycle, no? Pain comes, pain goes. But the heart… the heart remembers. Maybe the body is whispering before it screams. Listen. Not to fear, but to truth. 🌿
Himmat Singh
December 25, 2025 AT 02:19The assertion that 70–80% of patients can be ruled out within two hours is misleading. The sensitivity of high-sensitivity troponin assays varies significantly across populations, and false negatives remain a documented clinical risk, particularly in elderly patients with renal impairment. The data cited lacks context.