When someone is diagnosed with celiac disease, the focus usually lands on stomach pain, bloating, diarrhea, or weight loss. But there’s another part of the body that often gets overlooked - the liver. Up to 40% of people with untreated celiac disease show abnormal liver enzyme levels, even when they have no signs of liver trouble. And here’s the surprising part: for most of them, those liver numbers go back to normal - not with medication, but simply by cutting out gluten.
Why Does Celiac Disease Affect the Liver?
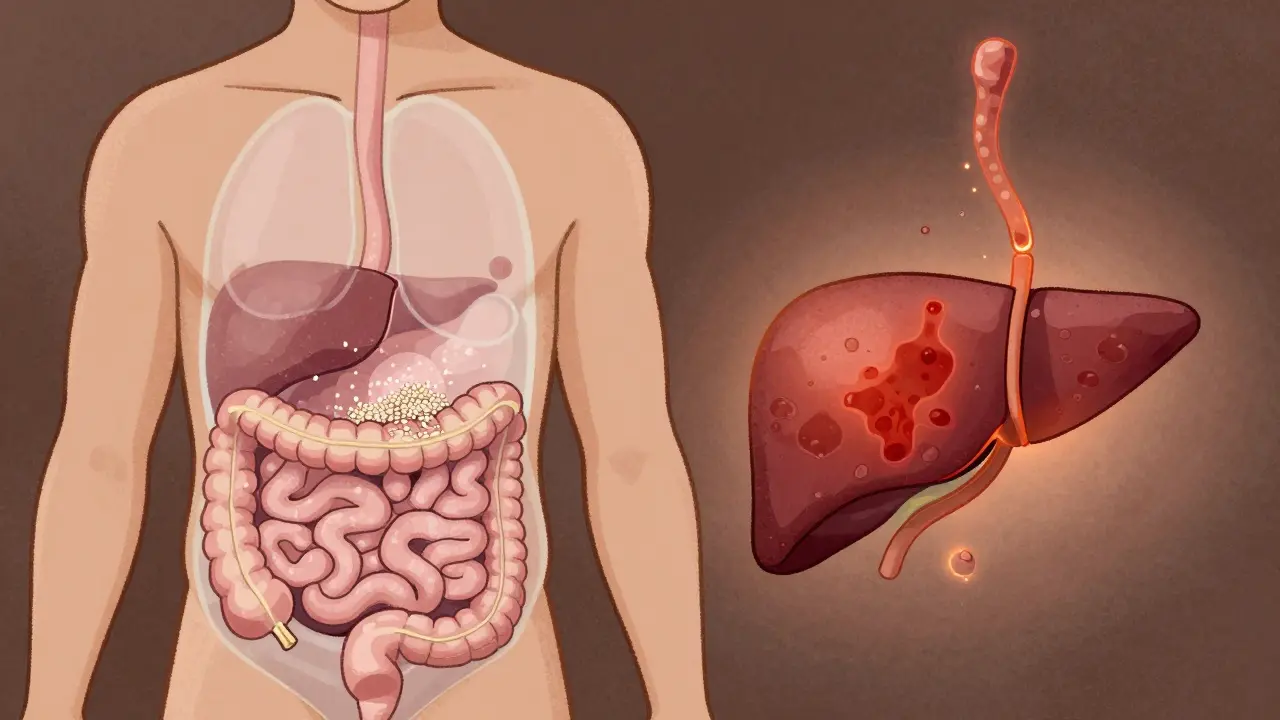
Celiac disease isn’t just a gut problem. It’s an autoimmune condition where the body attacks its own tissues after eating gluten. That attack mainly targets the small intestine, but the immune system doesn’t stop there. It can turn on other organs, including the liver. The connection isn’t random. It’s rooted in biology. One major reason is increased intestinal permeability - often called "leaky gut." When gluten damages the lining of the small intestine, undigested particles and toxins slip through into the bloodstream. The liver, as the body’s main filter, gets flooded with these unwanted substances. Over time, that constant exposure triggers inflammation. Studies show this process leads to fatty deposits, swelling, and even early scarring in the liver. Another factor is autoimmune cross-reactivity. The immune system, already confused by gluten, sometimes mistakes liver cells for foreign invaders. This is why celiac disease often shows up alongside autoimmune liver diseases like autoimmune hepatitis or primary biliary cholangitis. In fact, 4 to 6.4% of people diagnosed with autoimmune hepatitis also have undiagnosed celiac disease. Then there’s malabsorption. Damaged intestines can’t absorb key nutrients - especially fat-soluble vitamins like A, D, E, and K. These vitamins play a protective role in liver health. Without them, the liver becomes more vulnerable to damage. Low vitamin E, for example, has been linked to increased oxidative stress in liver cells.What Do Liver Abnormalities Look Like in Celiac Patients?
The most common sign is elevated liver enzymes, specifically ALT (alanine aminotransferase) and AST (aspartate aminotransferase). These are proteins released when liver cells are injured. In celiac disease, they’re usually only mildly to moderately high - often two to five times the normal upper limit. That’s not enough to trigger alarm bells in many clinics, which is why liver issues in celiac patients often go unnoticed. A 2007 study of 67 biopsy-confirmed celiac patients found:- 70.1% had both ALT and AST elevated
- 20.9% had only ALT high
- 9% had only AST high
Gluten-Free Diet: The Unexpected Liver Treatment
The most powerful tool for fixing liver problems in celiac disease isn’t a pill - it’s a dietary change. Multiple studies confirm that strict, long-term gluten-free diet adherence reverses liver damage in most cases. Dr. Daniel Leffler’s research at Beth Israel Deaconess Medical Center tracked 100 celiac patients with elevated liver enzymes. After 12 to 18 months on a gluten-free diet, 79% saw their liver numbers return to normal. Another study found that 85% normalized within 12 months. What’s remarkable is that this happens without liver-specific drugs. The liver heals itself once the trigger - gluten - is removed. The inflammation drops, fat deposits shrink, and enzyme levels fall. In some cases, liver biopsies taken before and after a gluten-free diet show near-complete restoration of healthy tissue. But here’s the catch: not everyone gets better. If liver enzymes stay high after a year of strict gluten avoidance, doctors need to look for other causes. That’s when they test for autoimmune hepatitis, primary biliary cholangitis, or MASLD unrelated to celiac disease. About 4 to 6.4% of celiac patients with persistent liver issues have a coexisting autoimmune liver condition that needs separate treatment.
The Hidden Risk: Gluten-Free Diet Can Worsen Fatty Liver
There’s a dark twist to this story. While cutting out gluten helps the liver, many gluten-free products are loaded with sugar, refined starches, and unhealthy fats. Rice flour, potato starch, corn syrup - these are common in gluten-free breads, crackers, and pastries. They spike blood sugar and promote fat storage in the liver. This creates a paradox: the treatment for celiac disease might accidentally cause MASLD. Studies show that celiac patients on a standard gluten-free diet are more likely to gain weight and develop fatty liver than those who eat whole, unprocessed foods. A 2023 study from the Celiac Disease Foundation found that patients who worked with a registered dietitian specializing in celiac disease normalized their liver enzymes 30% faster than those who just followed generic gluten-free advice. Why? Because the dietitians pushed for:- Fruits, vegetables, and legumes
- Lean proteins like chicken, fish, and eggs
- Whole gluten-free grains like quinoa, buckwheat, and brown rice
- Healthy fats from nuts, seeds, and olive oil
- Avoiding packaged snacks and sugary cereals
When Should You Get Your Liver Checked?
If you’ve just been diagnosed with celiac disease, your doctor should already be checking your liver enzymes. But if they aren’t - ask for it. A simple blood test for ALT, AST, and ALP can catch problems early. Current guidelines recommend:- Testing liver enzymes at diagnosis
- Rechecking every 3 to 6 months until levels normalize
- If enzymes stay high after 12 months, testing for autoimmune liver diseases
What’s Next in Research?
Scientists are digging deeper. Researchers at the University of Helsinki are tracking 500 celiac patients over 10 years to see if longer gluten exposure leads to worse liver damage. Meanwhile, the Mayo Clinic is studying genetic markers. Early data suggests people with two copies of the HLA-DQ2 gene (homozygous) are 2.3 times more likely to develop liver abnormalities than those with just one copy. Pharmaceutical companies are also stepping in. Takeda Pharmaceutical completed a Phase II trial in late 2023 testing an enzyme therapy designed to break down gluten in the gut before it triggers immune reactions. If successful, it could reduce not just gut damage, but also liver inflammation. The diagnostic market for celiac-related liver issues is growing fast. In 2015, only 65% of celiac workups included liver tests. By 2024, that number jumped to 92%. More doctors are waking up to the connection.What Patients Are Saying
Online forums are full of stories like this one from Reddit user u/CeliacForLife (March 2023): "My ALT was 142 when I was diagnosed. Doctors thought it was fatty liver from being overweight. Then they found my tTG antibodies. I went gluten-free. Six months later, my ALT was 32. No meds. Just food." A 2022 survey by BeyondCeliac.org found that 68% of celiac patients with liver abnormalities had never heard of the link before their diagnosis. Most didn’t feel sick - the only clue was a blood test result they didn’t understand. The message is clear: if you have celiac disease, your liver matters. And if you have unexplained liver problems, celiac disease might be the hidden cause.Key Takeaways
- Between 15% and 40% of untreated celiac patients have elevated liver enzymes.
- Most liver abnormalities improve or disappear within 12 to 18 months on a strict gluten-free diet.
- Autoimmune hepatitis and MASLD are common coexisting conditions.
- Processed gluten-free foods can worsen fatty liver - choose whole foods instead.
- Always test liver enzymes at celiac diagnosis and recheck regularly.
- If liver enzymes stay high after a year, check for autoimmune liver disease.
- Screening for celiac disease is now recommended for people with unexplained cirrhosis.

jenny guachamboza
December 23, 2025 AT 04:37Gabriella da Silva Mendes
December 23, 2025 AT 23:46Nader Bsyouni
December 24, 2025 AT 01:06Ajay Brahmandam
December 24, 2025 AT 05:24Aliyu Sani
December 26, 2025 AT 05:05Tony Du bled
December 27, 2025 AT 19:30Candy Cotton
December 27, 2025 AT 21:35Tarun Sharma
December 29, 2025 AT 06:50Jim Brown
December 29, 2025 AT 12:09Sam Black
December 31, 2025 AT 07:01Cara Hritz
January 1, 2026 AT 22:38Jamison Kissh
January 3, 2026 AT 22:15Art Van Gelder
January 5, 2026 AT 13:32Kathryn Weymouth
January 6, 2026 AT 20:21Julie Chavassieux
January 7, 2026 AT 10:08