CNS Depressant Combination Risk Calculator
Your Cannabis Use
Other Depressant
Your Risk Assessment
Warning: You're at significant risk of additive sedation. Stop immediately and contact medical professionals if you experience any symptoms.
Urgent Medical Attention Required: Symptoms include slow breathing (fewer than 8 breaths per minute), bluish lips, or inability to wake up. Call emergency services immediately.
Combining cannabis with other central nervous system (CNS) depressants isn’t just a bad idea-it’s dangerous. If you’re using prescription sleep aids, anti-anxiety meds like Xanax or Valium, opioids for pain, or even alcohol, adding cannabis can push your body into a state no one plans for: extreme drowsiness, slowed breathing, memory blackouts, or worse. This isn’t theoretical. Emergency rooms across the U.S. and Australia are seeing more cases every year, and the science is clear: the effects aren’t just added together-they multiply.
How Cannabis Acts as a CNS Depressant
Many people think of cannabis as a stimulant because of the energy or laughter it sometimes brings. But that’s usually from low doses or high-CBD strains. At moderate to high doses, especially with THC levels above 10%, cannabis acts as a CNS depressant. It slows down brain activity by binding to CB1 receptors, which are densely packed in areas controlling movement, memory, and breathing. This is similar to how benzodiazepines and barbiturates work-except instead of boosting GABA, cannabis tweaks the endocannabinoid system. The result? Slowed reaction time, poor coordination, confusion, and drowsiness.
When smoked or vaped, these effects hit fast-within minutes-and peak around 30 minutes. Edibles take longer, often 1 to 3 hours to kick in, but they last much longer, sometimes up to 8 hours. That’s important. If you take a pill for anxiety at 8 a.m. and eat a gummy at noon, you’re not just adding two effects-you’re stacking them over time. And the longer they overlap, the higher the risk.
Why the Combination Is So Risky
Here’s the core problem: both cannabis and other CNS depressants suppress breathing. Not just a little-enough to be life-threatening. Opioids like oxycodone or fentanyl reduce the brain’s drive to breathe. Cannabis does the same, but through different pathways. When you combine them, the suppression isn’t 1+1=2. It’s closer to 1+1=3 or 4. That’s called synergistic depression.
Studies show people using both cannabis and benzodiazepines are over three times more likely to end up in the emergency room than those using only the prescription drug. In 67% of those cases, the main issue was low oxygen levels. One patient in a 2023 case report took half a milligram of Xanax and one hit of 20% THC flower. He woke up on the bathroom floor six hours later, with oxygen saturation at 82%. Normal is 95% or higher. That’s a medical emergency.
Even in controlled medical settings, the risks are real. Anesthesiologists at Washington University found that cannabis users needed 20-25% more propofol to get the same level of sedation during surgery-but then had 37% more breathing problems after. That means doctors can’t predict how someone will react. What works for one person might nearly stop another’s breathing.
Who’s Most at Risk
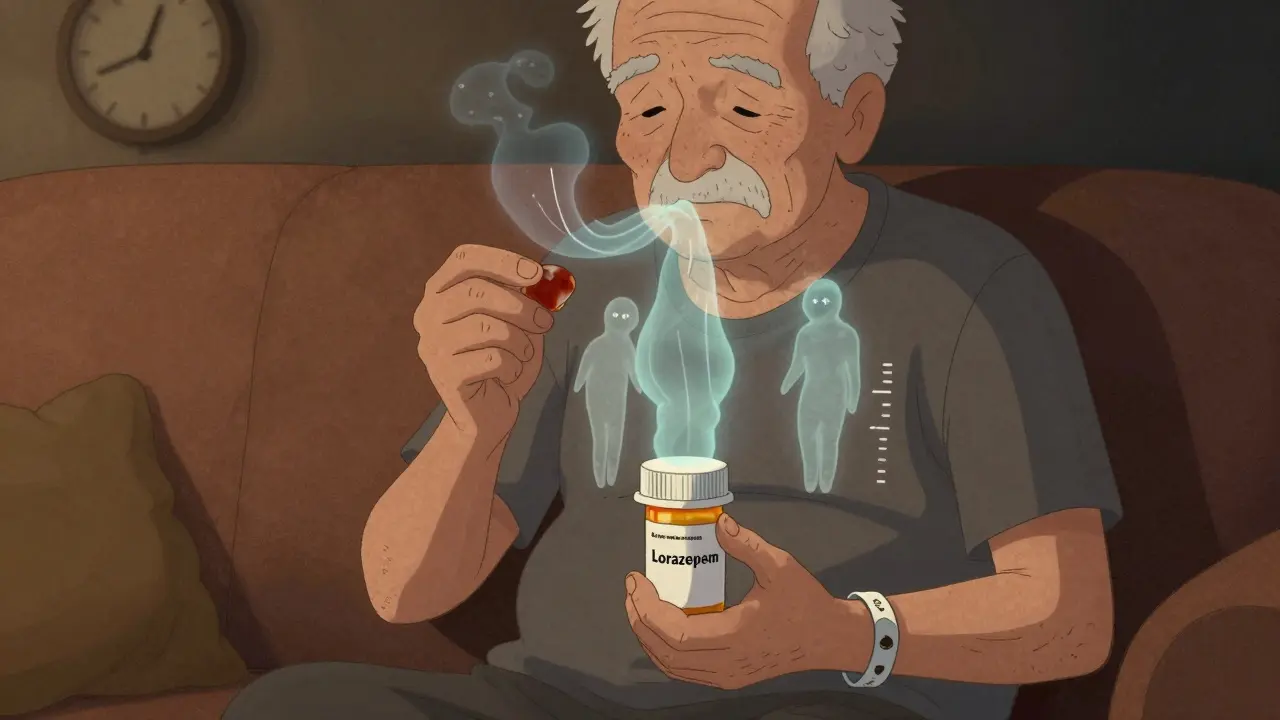
It’s not just recreational users. Older adults are especially vulnerable. Many take opioids for chronic pain, benzodiazepines for insomnia or anxiety, and then turn to cannabis because they’ve heard it’s “natural.” But aging changes how the body processes drugs. Liver function slows. Fat tissue holds onto THC longer. The brain becomes more sensitive to sedation. A 70-year-old using 5mg of THC with a low-dose lorazepam might not feel “high,” but their breathing could still be dangerously suppressed.
People with existing lung or heart conditions are also at higher risk. If your body already struggles to get enough oxygen, adding a depressant that slows breathing is like turning down the air supply on a fire that’s barely burning.
And it’s not just prescription drugs. Over-the-counter sleep aids, antihistamines like diphenhydramine (Benadryl), and even some cold medicines contain CNS depressants. Mixing those with cannabis is just as risky. A 2022 survey of over 1,200 medical cannabis users found that nearly 25% had experienced an episode of extreme sedation so bad they needed medical help.
What the Experts Say
Major medical groups are sounding the alarm. The American Society of Anesthesiologists says anyone using cannabis within 72 hours of surgery needs close monitoring. The FDA updated labels on all prescription CNS depressants in 2022 to include warnings about cannabis. The European Medicines Agency now requires the same on all medical cannabis products sold in Europe.
Dr. Igor Grant from UC San Diego calls this one of the most under-recognized risks in modern medicine. “We’re seeing patients on multiple medications, thinking cannabis is safe because it’s plant-based,” he said in a 2021 testimony. “But the brain doesn’t care if a drug comes from a lab or a plant. It only cares about the receptors it hits.”
Even in places where medical cannabis is legal, doctors are being trained. California now requires all physicians who certify patients for cannabis to complete a 2-hour course on drug interactions. Since the rule started in 2022, high-risk combinations have dropped by 28%.
Safe Alternatives and Risk Reduction
If you’re on a CNS depressant and want to try cannabis, don’t just assume it’s fine. Here’s what the evidence says about reducing risk:
- Avoid high-THC products. Stick to strains or products under 10% THC. Above that, the sedative and cognitive risks jump sharply.
- Choose CBD-dominant products. A 2022 JAMA study showed that high-CBD, low-THC oil (150mg CBD, less than 0.3% THC) had no significant interaction with alprazolam. CBD doesn’t bind strongly to CB1 receptors, so it doesn’t cause the same depressant effects.
- Space out doses. If you must use both, wait at least 4 hours between taking a depressant and cannabis. This reduces overlap and gives your body time to metabolize one before introducing the other.
- Start low and go slow. Even if you’ve used cannabis before, your sensitivity changes when you’re on other meds. Try 2.5mg of THC or less. Wait 2 hours. Don’t take more.
- Talk to your doctor. Don’t hide your cannabis use. Tell them what you’re taking, how much, and how often. They can adjust your prescription or suggest alternatives.
Some patients have successfully reduced opioid use by adding low-dose THC under strict supervision. In one 2022 study, 15 chronic pain patients cut their opioid doses by nearly half without serious side effects. But that was done in a controlled clinic with daily monitoring. This isn’t something to try at home.

What to Do If You’ve Already Combined Them
If you’ve taken cannabis with a CNS depressant and feel extremely drowsy, confused, or have trouble breathing, don’t wait. Call emergency services immediately. Don’t assume you’ll “sleep it off.” Respiratory depression can happen silently, without vomiting or obvious signs.
If you’re caring for someone who’s using both, keep an eye on their breathing. Look for slow, shallow breaths-less than 8 per minute. Check their lips or fingertips for bluish color. If you see that, it’s time to act.
Keep naloxone on hand if opioids are involved. While naloxone doesn’t reverse cannabis effects, it can counteract opioid-induced breathing problems and buy time until help arrives.
The Bottom Line
Cannabis isn’t a magic bullet. It’s a powerful drug with real, measurable effects on the brain and body. When mixed with other CNS depressants, those effects become unpredictable and potentially deadly. There’s no safe threshold for combining them without medical oversight. The idea that “it’s natural, so it’s safe” is dangerous and false.
If you’re using any prescription sedative, painkiller, or sleep aid, talk to your doctor before using cannabis-even if it’s legal. If you’re using cannabis and feel unusually tired, foggy, or short of breath, stop and reassess. Your life isn’t worth the gamble.
Can CBD interact with CNS depressants the same way THC does?
No, CBD doesn’t interact the same way. Unlike THC, CBD doesn’t strongly bind to CB1 receptors in the brain, so it doesn’t cause sedation or respiratory depression on its own. A 2022 JAMA study found that high-CBD, low-THC cannabis oil (150mg CBD, under 0.3% THC) had no significant interaction with alprazolam. That said, CBD can affect how the liver processes some medications, so it’s still important to check with your doctor before combining it with any prescription drug.
Is it safe to use cannabis with alcohol?
No. Alcohol is a CNS depressant, and combining it with cannabis increases sedation, dizziness, and the risk of vomiting or choking. Studies show people who use both are more likely to have accidents, blackouts, and impaired judgment. The combination also raises the risk of respiratory depression, especially in larger doses. There’s no safe level of mixing alcohol and cannabis.
How long should I wait after using cannabis before taking a benzodiazepine?
Wait at least 4 hours after using cannabis before taking a benzodiazepine, and vice versa. This reduces the chance of overlapping peak effects. If you smoked or vaped, wait 4 hours. If you ate an edible, wait 6-8 hours because it takes longer to peak and lasts much longer. Even then, start with the lowest possible dose of the prescription drug. Never assume you’re “used to it”-your tolerance changes when other drugs are in your system.
Can I use cannabis instead of my anxiety or sleep medication?
Don’t stop your prescribed medication without talking to your doctor. While some people find cannabis helps with anxiety or sleep, it’s not a proven replacement for benzodiazepines or sleep aids. Cannabis can cause rebound anxiety, worsen sleep quality over time, and lead to dependence. If you want to switch, work with your doctor on a gradual, monitored plan-not by self-medicating.
Are there any warning signs I should watch for?
Yes. Watch for extreme drowsiness, confusion, slurred speech, slow or shallow breathing (fewer than 8 breaths per minute), bluish lips or fingernails, inability to wake up, or memory loss after using both substances. If you or someone else shows these signs, call emergency services immediately. Don’t wait to see if it gets better-it might not.

lokesh prasanth
January 20, 2026 AT 14:38MARILYN ONEILL
January 21, 2026 AT 08:46Yuri Hyuga
January 22, 2026 AT 12:02Rod Wheatley
January 24, 2026 AT 10:51Roisin Kelly
January 25, 2026 AT 16:33Jerry Rodrigues
January 27, 2026 AT 05:19Jarrod Flesch
January 27, 2026 AT 07:49Samuel Mendoza
January 27, 2026 AT 23:53Glenda Marínez Granados
January 28, 2026 AT 03:20Malvina Tomja
January 29, 2026 AT 16:47