Amiodarone is one of the most powerful drugs doctors use to treat dangerous heart rhythm problems. But it’s not the only option. When someone has atrial fibrillation, ventricular tachycardia, or other life-threatening arrhythmias, choosing the right antiarrhythmic drug isn’t just about effectiveness-it’s about safety, long-term risks, and how the body handles the drug over time. Many patients and even some clinicians still think amiodarone is the go-to because it works well. But it’s not always the best choice. Here’s what really happens when you compare it to other drugs in the same class.
Why Amiodarone Stands Out
Amiodarone works differently from most other antiarrhythmic drugs. While others target one specific ion channel in heart cells, amiodarone affects sodium, potassium, and calcium channels all at once. This broad action makes it effective against many types of irregular heartbeats, including ones that other drugs fail to control. In clinical trials, amiodarone reduces the risk of sudden cardiac death by about 20% compared to placebo in high-risk patients, especially after a heart attack. That’s why it’s still used in hospitals for emergencies and in patients who haven’t responded to anything else.
But here’s the catch: amiodarone stays in your body for months-even years-after you stop taking it. That’s because it’s highly fat-soluble and builds up in organs like the liver, lungs, and thyroid. This long half-life means it works for a long time, but it also means side effects can show up slowly and stick around. A 2023 study in the Journal of the American College of Cardiology found that nearly 40% of patients on long-term amiodarone developed thyroid dysfunction, and 15% had lung changes visible on scans.
How Other Antiarrhythmic Drugs Compare
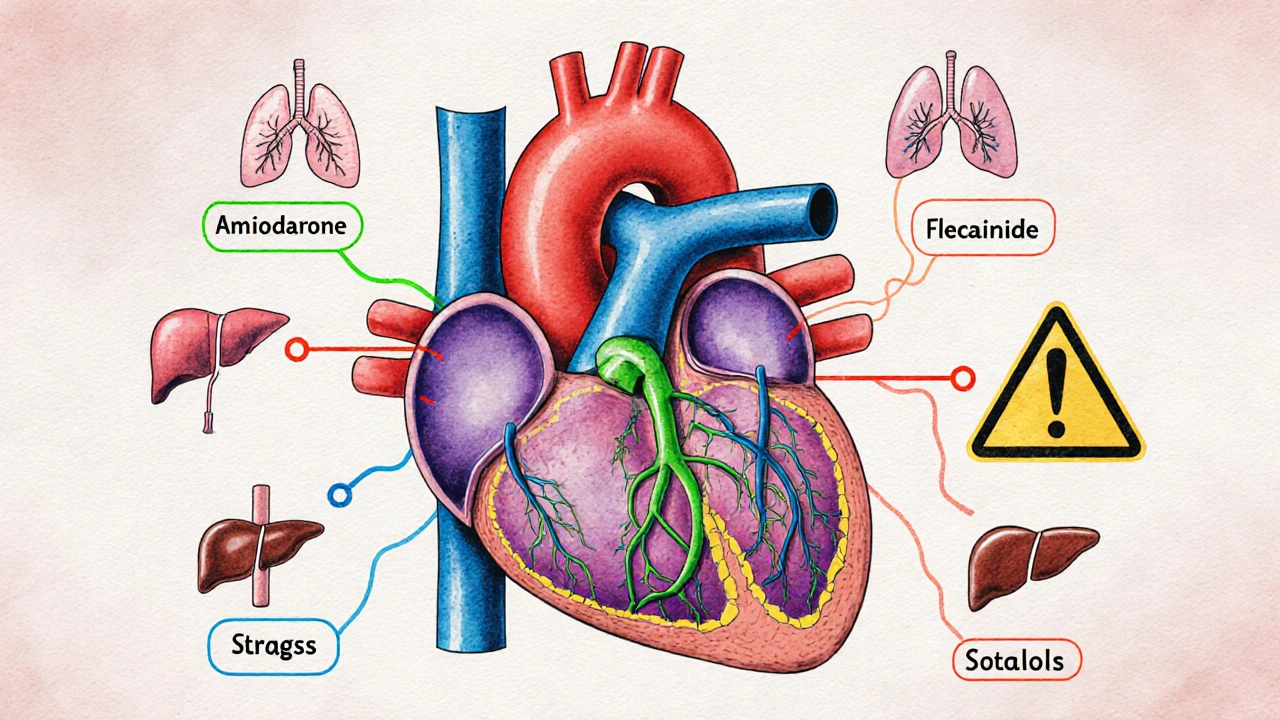
There are four main classes of antiarrhythmic drugs, and each has different uses and risks. Amiodarone is in Class III, which means it blocks potassium channels. But other classes include drugs like flecainide (Class Ic), sotalol (Class III), and dofetilide (Class III). Let’s break down how they stack up.
| Drug | Class | Primary Use | Effectiveness | Major Risks | Monitoring Needed |
|---|---|---|---|---|---|
| Amiodarone | III | VT, AFib, post-MI | High | Lung toxicity, thyroid issues, liver damage, vision changes | Every 6 months: LFTs, TFTs, chest X-ray, eye exam |
| Flecainide | Ic | AFib in structurally normal hearts | Moderate | Proarrhythmia, especially after heart attack | ECG before and after starting |
| Sotalol | III | AFib, VT | Moderate to high | QT prolongation, torsades de pointes | ECG daily for first 3 days, electrolytes |
| Dofetilide | III | AFib, atrial flutter | Moderate | QT prolongation, requires hospital initiation | ECG, creatinine, hospital admission |
| Propafenone | Ic | AFib in healthy hearts | Moderate | Proarrhythmia, bronchospasm, dizziness | ECG, liver function |
Unlike amiodarone, drugs like flecainide and propafenone are much safer for younger patients with no heart damage-but they’re dangerous if you’ve had a heart attack or heart failure. That’s why they’re never used in people with structural heart disease. Sotalol and dofetilide are safer for the lungs and thyroid, but they carry a risk of torsades de pointes, a dangerous type of ventricular arrhythmia. That means patients need to start these drugs in the hospital with continuous ECG monitoring.
When Amiodarone Is the Right Choice
Amiodarone isn’t a first-line drug for most people. But there are clear situations where it’s the best or only option. If you’ve had a heart attack and your heart is weakened, and other drugs have failed, amiodarone may be the only one that keeps you alive. It’s also used in patients with severe atrial fibrillation who can’t tolerate beta-blockers or calcium channel blockers. In Australia, the Therapeutic Goods Administration (TGA) recommends amiodarone as a second-line agent for persistent AFib when rhythm control is needed and other drugs aren’t working.
It’s also used in patients with implanted defibrillators who keep getting shocks. Studies show amiodarone can reduce those shocks by up to 50%. That’s a huge quality-of-life improvement. For these patients, the long-term risks are weighed against the constant danger of sudden cardiac arrest.
The Hidden Costs of Amiodarone
Most people don’t realize how much monitoring amiodarone requires. It’s not just a pill you take once a day and forget about. You need regular blood tests for liver and thyroid function. Every six months, you need a chest X-ray or CT scan to check for lung scarring. Eye exams are needed because amiodarone can cause corneal deposits-harmless in most cases, but they can blur vision. And if you’re over 60, your risk of developing hypothyroidism jumps to over 25%.
These aren’t rare side effects. They’re common. And they’re often missed. A 2024 audit of 500 patients on long-term amiodarone in Melbourne found that 62% hadn’t had a thyroid test in over a year. Many patients were told to see their GP, but without specific guidance, those tests got dropped. That’s why it’s critical to have a cardiologist managing this drug-not just a general practitioner.
Alternatives That Are Often Overlooked
Many patients assume they have to choose between amiodarone and nothing. But there are other paths. Catheter ablation has become much more effective in recent years. For atrial fibrillation, success rates now exceed 70% in patients without advanced heart disease. That means many people can get rid of their arrhythmia without lifelong pills.
For those who still need medication, dronedarone (a derivative of amiodarone) is an option. It’s less effective but has far fewer lung and thyroid side effects. The problem? It doesn’t work for everyone. In fact, it’s not recommended for patients with heart failure or permanent AFib. Still, for younger patients with paroxysmal AFib, it’s a good middle ground.
And then there’s the role of lifestyle. Weight loss, sleep apnea treatment, and reducing alcohol intake can significantly reduce arrhythmia burden-even in patients on amiodarone. A 2025 study in The Lancet showed that obese patients with AFib who lost 10% of their body weight had a 60% lower chance of recurrence, even without changing their meds.

What Doctors Wish Patients Knew
Most cardiologists don’t start patients on amiodarone unless they’ve tried at least two other drugs. It’s not because they’re being cautious-it’s because the side effects are real, slow to appear, and sometimes irreversible. If you’re on amiodarone, you need to know: this isn’t a short-term fix. You’re signing up for lifelong monitoring. And if you’re not getting regular tests, you’re at risk.
Also, don’t assume that because it’s a powerful drug, it’s the best. For many people, a simpler drug like sotalol, combined with ablation, is a better long-term strategy. Amiodarone isn’t the hero-it’s the last resort. And that’s okay. But it needs to be used with eyes wide open.
When to Ask for a Second Opinion
If your doctor prescribes amiodarone without discussing alternatives, or if you’ve been on it for more than six months without any monitoring, it’s time to ask questions. Ask for a referral to an electrophysiologist-a heart rhythm specialist. Ask about ablation. Ask about dronedarone. Ask about lifestyle changes that could reduce your need for meds.
There’s no shame in seeking a second opinion. Arrhythmias are complex. Medications have trade-offs. And you deserve to know all your options before committing to a drug that stays in your body for years.
Is amiodarone the most effective antiarrhythmic drug?
Yes, in terms of stopping arrhythmias, amiodarone is one of the most effective. It works where other drugs fail, especially in patients with heart damage. But effectiveness doesn’t mean safety. Its long-term side effects make it a last-resort option for many patients.
Can you take amiodarone forever?
Some people do take it for years, but it’s not recommended without strict monitoring. The risk of lung, liver, and thyroid damage increases the longer you’re on it. Many doctors try to reduce the dose over time or switch to another drug if the arrhythmia is under control.
What are the safest alternatives to amiodarone?
For patients with healthy hearts, flecainide or propafenone are safer. For those with heart disease, sotalol or dofetilide may be options, but they require hospital monitoring. Dronedarone is a milder version of amiodarone with fewer side effects, but it’s not for everyone. Ablation is often the safest long-term solution for AFib.
Why does amiodarone cause thyroid problems?
Amiodarone contains iodine-about 37% of its weight. That’s 10 times more iodine than the daily recommended intake. Too much iodine can overstimulate or suppress the thyroid gland, leading to either hyperthyroidism or hypothyroidism. This is why thyroid function tests are mandatory every 6 months.
Can amiodarone damage your lungs?
Yes. Amiodarone can cause interstitial lung disease, which leads to scarring and breathing problems. It’s rare but serious. Symptoms include dry cough, shortness of breath, and fatigue. A chest CT scan can detect early changes. If caught early, stopping the drug can prevent permanent damage.
How often should you get blood tests on amiodarone?
Every 6 months: liver enzymes, thyroid function (TSH, free T4), and electrolytes. An annual chest X-ray or low-dose CT scan is recommended. Eye exams should be done every 12 months. Skipping these tests increases the risk of irreversible damage.
What to Do Next
If you’re on amiodarone, make sure you’re getting the right tests. If you’re considering it, ask about ablation and other drugs first. Don’t accept it as the only option. Arrhythmias are treatable-but the best treatment isn’t always the strongest drug. It’s the one that gives you the best chance at a long, healthy life without constant side effects.

Abdula'aziz Muhammad Nasir
November 18, 2025 AT 11:52Amiodarone is a double-edged sword. I've seen patients on it for years with no monitoring-some end up with pulmonary fibrosis and never knew why. The real issue isn't the drug, it's the system that lets GPs prescribe it without follow-up. Cardiologists know this. Primary care? Not so much. If you're on this, demand a rhythm specialist. Not a suggestion-a requirement.
Arun Mohan
November 19, 2025 AT 01:06Look, I get it. Amiodarone's got baggage. But let’s be real-most of these ‘alternatives’ are just fancy placebos for people who don’t want to face the truth: sometimes the only thing standing between you and sudden death is a toxic, slow-burning chemical that turns your body into a science experiment. If you’re alive because of it, stop complaining about thyroid levels. You’re lucky.
Jeff Moeller
November 20, 2025 AT 00:44It’s not about which drug is strongest-it’s about which one lets you live without becoming a ghost of yourself. Amiodarone doesn’t cure arrhythmias. It just buys time. And time is the one thing you can’t get back once your lungs are scarred or your thyroid is kaput. We treat symptoms like they’re the enemy. But the real enemy is the illusion that medicine can fix everything without cost.
Jessica Engelhardt
November 21, 2025 AT 11:22So let me get this straight-we’re supposed to trust a drug that’s basically liquid iodine with a side of lung cancer? And this is what American medicine calls innovation? I mean, sure, it works. But so does a tourniquet. That doesn’t mean you strap one on for life. Someone’s gotta ask: why are we still using a 1960s drug in 2025? Because Big Pharma likes the profit margin? Just say it.
Tara Stelluti
November 22, 2025 AT 22:27I was on amiodarone for 18 months. My doctor said ‘it’s fine.’ I got dizzy, my eyes burned, I couldn’t breathe after walking up stairs. I asked for a CT scan. They said ‘it’s not necessary.’ Two months later I had lung fibrosis. Now I’m on oxygen. Don’t let this happen to you. If your doctor won’t listen, fire them. I did. And I’m still alive. Barely.
Margaret Wilson
November 23, 2025 AT 19:07Amiodarone: the drug that gives you a heartbeat but steals your lungs, thyroid, liver, and soul 😔🩺💔
Brad Samuels
November 23, 2025 AT 20:31There’s something deeply human about this whole conversation. We’re not just talking about drugs-we’re talking about how we value life. Do we want to live longer, even if we’re barely alive? Or do we want to live well, even if it means taking a risk? Amiodarone forces that question on you. No sugarcoating. No easy answers. Just you, your body, and the silence after the last heartbeat.
Herbert Scheffknecht
November 24, 2025 AT 13:26People think drugs are magic bullets. They’re not. They’re trade-offs written in blood and biopsy results. Amiodarone doesn’t fix your heart-it buys you time to fix your life. That’s why ablation matters. That’s why weight loss matters. That’s why asking for a second opinion isn’t weakness-it’s the only sane thing you can do when medicine hands you a grenade and says ‘take it, we’ll watch.’
Tyrone Luton
November 24, 2025 AT 20:26You know what’s more dangerous than amiodarone? The arrogance of doctors who think they know what’s best without listening. I had a patient-62, diabetic, sedentary, drank two bottles of wine a night. They put her on amiodarone and told her to ‘just take it.’ She didn’t get an echo, didn’t get a thyroid test, didn’t get lifestyle advice. She died of pulmonary fibrosis three years later. The chart said ‘sudden cardiac arrest.’ The truth? It was neglect dressed up as treatment.
Amiodarone isn’t the villain. The system is.
william volcoff
November 24, 2025 AT 23:36For what it’s worth-I’m a cardiologist. I’ve prescribed amiodarone. I’ve also watched patients turn into walking side effect lists. Here’s the truth no one says out loud: if you’re young, healthy, and have paroxysmal AFib, ablation should be your first option, not your last. Amiodarone is for when everything else failed. Not because it’s better. Because we’re scared to admit we don’t have a better answer yet.
And yes-dronedarone is underrated. It’s not magic, but it’s not poison either. Give it a shot before you sign up for a lifetime of scans.
Danielle Mazur
November 26, 2025 AT 17:55Amiodarone was developed during the Cold War. The U.S. military tested it on soldiers to stabilize heart rhythms under extreme stress. Then it got approved for civilians. No long-term studies. No transparency. Now it’s everywhere. And no one talks about the fact that the iodine in it came from a Soviet-era chemical process. Coincidence? Or was this always meant to be a slow-acting control mechanism? Just saying.